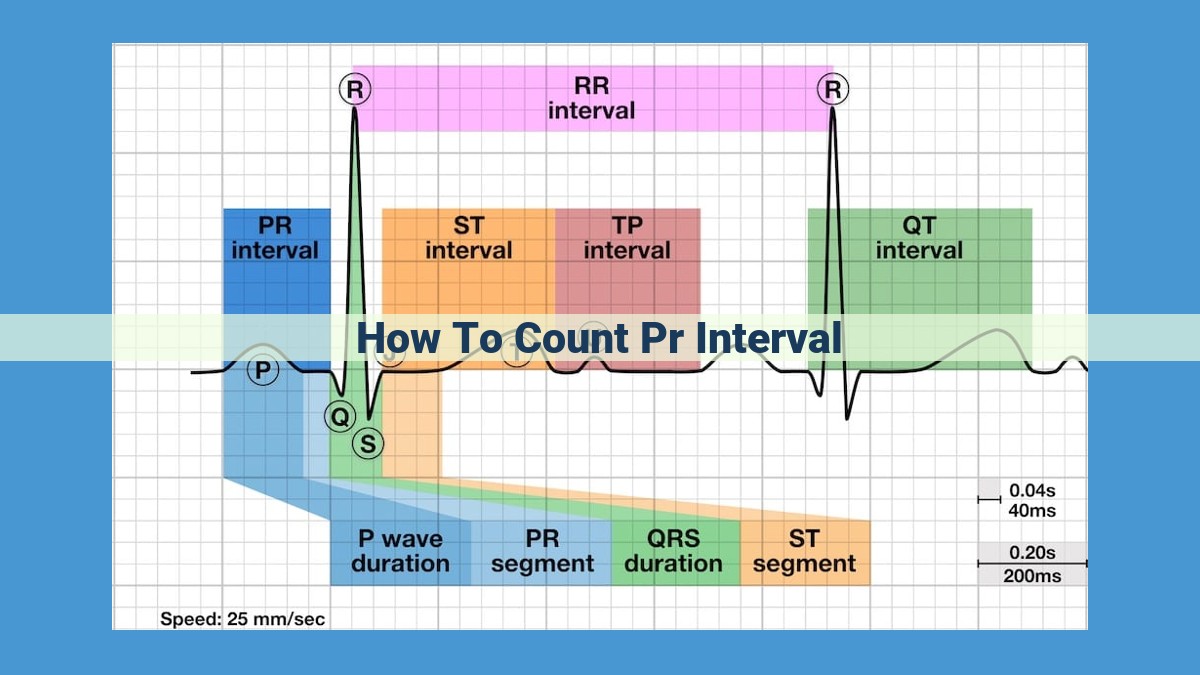
To count the PR interval, start by identifying the P wave, characterized by its rounded morphology and preceding the QRS complex. Locate the R wave, the largest deflection in the QRS. Measure the distance between the onset of the P wave and the onset of the R wave using calipers or another tool. Express the result in milliseconds, adhering to ECG standardization conventions. Variations in the PR interval can provide insights into cardiac rhythm and conduction abnormalities.
Identifying the P Wave: Unlocking the Key to PR Interval Measurement
In the realm of electrocardiography (ECG), the P wave stands as a crucial foundation for accurately measuring the PR interval, a vital indicator of cardiac health. Identifying the P wave is paramount, as it marks the onset of electrical activity in the heart’s atria.
Distinctive Characteristics of the P Wave
The P wave is often described as a small, rounded deflection that precedes the QRS complex. It typically has a duration of 0.08-0.1 seconds and an amplitude of 0.1-0.25 mV. The P wave’s positive deflection indicates the spread of electrical impulses from the sinoatrial (SA) node, located in the right atrium, across both atria.
Recognizing Variations in P Wave Morphology
While the P wave typically follows a consistent pattern, it can exhibit variations in shape and amplitude depending on lead placement. In lead II, the P wave is often upright and narrow, while in lead V1, it may appear biphasic, with both positive and negative deflections. Variations in amplitude can also occur, with the P wave appearing larger in leads close to the atria, such as lead V1.
Optimal Lead Placement for Clear P Wave Visualization
For accurate interpretation of the P wave, choosing the optimal lead placement is essential. Lead II provides a clear view of the P wave’s morphology and timing, making it the preferred lead for rhythm interpretation. Additionally, leads V1 and V2 can be useful for identifying P waves that are obscured by the QRS complex in other leads.
Understanding the R Wave: The Heart of the PR Interval
In the realm of electrocardiography (ECG), the R wave stands as a vital component of the QRS complex, which represents the electrical depolarization of the ventricles. This integral wave holds the key to accurately measuring the PR interval, an essential parameter in rhythm interpretation.
Morphology and Characteristics of the R Wave
The R wave is the positive deflection or upward wave in the QRS complex. It follows the P wave, which represents atrial depolarization, and precedes the S wave. The R wave typically has the highest amplitude among all QRS deflections, reflecting the activation of a significant portion of the ventricular myocardium. Its shape and timing can vary depending on the ECG lead placement.
Distinguishing the R Wave from Other QRS Deflections
The QRS complex consists of multiple deflections, including the Q wave, R wave, S wave, and sometimes a T wave. The Q wave is a negative deflection that may precede the R wave, while the S wave is a negative deflection that follows the R wave.
The R wave is distinguished from other QRS deflections by its positive polarity and relatively large amplitude. It represents the peak of ventricular depolarization, when the electrical activation reaches the greatest number of myocardial cells.
Significance of R Wave Duration and Timing
The duration of the R wave provides valuable information about the electrical conduction within the ventricles. A prolonged R wave may indicate ventricular hypertrophy or conduction abnormalities, while a short R wave can be associated with certain arrhythmias.
The timing of the R wave relative to the P wave is crucial for measuring the PR interval. This interval represents the time it takes for the electrical impulse to travel from the atria (P wave) to the ventricles (R wave). Variations in the PR interval can indicate abnormalities in cardiac conduction, such as atrioventricular block.
Measuring the PR Interval: A Precise Quantifier of Heart Rhythms
In the electrocardiogram’s intricate symphony of waves, the PR interval stands as a crucial measure, revealing essential clues about the heart’s electrical activity. It’s a journey we embark on, starting with the P wave, the initial whisper of atrial depolarization. Like a conductor’s baton, it sets the stage for the heart’s rhythmic contractions.
The R wave, the boldest surge in the QRS complex, marks the moment when the impulse reaches the ventricles, the heart’s powerful pumping chambers. Their synchronized dance, from P to R, forms the PR interval, a silent yet potent indicator of the heart’s electrical harmony.
To accurately measure the PR interval, we arm ourselves with ECG calipers or other specialized tools. With meticulous precision, we navigate the EKG’s gridlines, tracing the distance between the P wave’s onset and the R wave’s peak. This seemingly simple measurement holds profound clinical significance.
Variations in the PR interval can hint at hidden cardiac ailments. A prolonged PR interval, for instance, may signal a block in the electrical pathway between the atria and ventricles, a condition known as heart block. Conversely, a shortened PR interval could indicate a condition called pre-excitation, where the electrical impulse finds an alternative route to the ventricles, bypassing the usual path.
Understanding the PR interval’s nuances empowers healthcare professionals to diagnose and manage heart rhythm disturbances effectively. It’s a testament to the power of precise measurement in unraveling the complexities of the human heart, guiding us towards optimal cardiac care.
Expressing the Measurement: Time Standardization in Electrocardiography
In the realm of electrocardiography, where interpreting the electrical activity of the heart is paramount, time standardization emerges as a crucial aspect of measurement accuracy. Electrocardiograms (ECGs) provide a graphical representation of the heart’s electrical impulses, allowing clinicians to assess its rhythm and electrical conduction.
One of the key parameters measured in ECG analysis is the PR interval, which represents the time delay between the onset of the P wave, signaling atrial depolarization, and the onset of the R wave, signifying the beginning of ventricular depolarization. To ensure consistency and comparability across different ECG recordings, the measurement of time intervals in electrocardiography is standardized to milliseconds.
When reporting PR interval durations, standardized conventions are followed. This ensures that measurements are comparable and reproducible among different healthcare professionals. The PR interval is typically expressed in milliseconds (ms), representing the duration of the electrical impulse’s travel from the atria to the ventricles.
By adhering to these time standardization protocols, clinicians can accurately quantify the PR interval and make informed clinical decisions based on its variations. Departing from these conventions can compromise the reliability and interpretability of ECG measurements, potentially leading to diagnostic errors and inappropriate patient management.
Therefore, healthcare professionals must be well-versed in the principles of time standardization in electrocardiography to ensure accurate and consistent PR interval measurements. By adhering to these standardized practices, they can enhance the quality of patient care and contribute to the advancement of cardiac diagnostics.