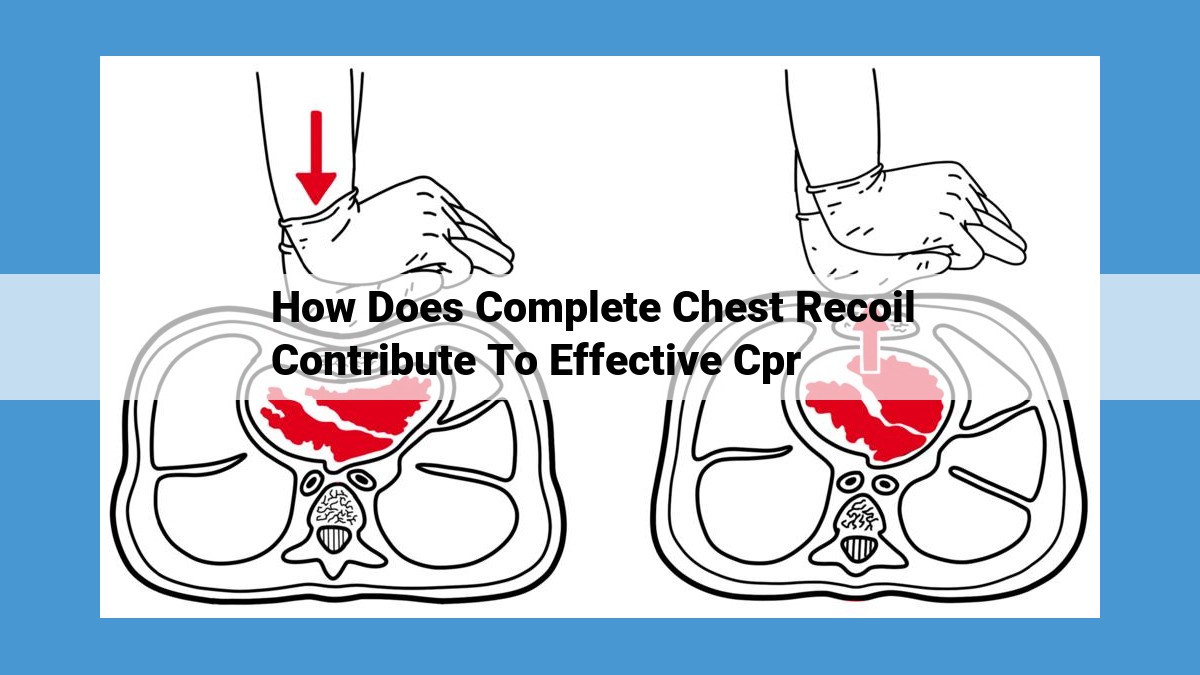
Complete chest recoil during CPR expands the lungs, enhancing ventilation and oxygenation. It also increases venous return to the heart, improving cardiac filling and output. Moreover, chest recoil facilitates increased coronary artery perfusion, supporting myocardial health. Additionally, it ensures efficient gas exchange, delivering oxygen to tissues and removing carbon dioxide. Importantly, it aids in effective defibrillation and restoration of spontaneous circulation.
The Vital Role of Chest Recoil in Optimal Lung Function
When it comes to the intricate machinery of life, our respiratory system plays a pivotal role. And within this system, the chest recoil mechanism is a silent maestro, ensuring that every breath we take is not just a simple act of inhalation and exhalation, but a symphony of physiological wonders.
Chest recoil is the elastic recoil force generated by the thoracic cage. As the diaphragm contracts and the external intercostal muscles pull the rib cage upward and outward, the lungs expand to accommodate the incoming air. But when the diaphragm relaxes and the external intercostal muscles cease their efforts, the thorax recoils, pushing the rib cage inward and downward. This recoil action is crucial for maintaining optimal lung function.
Complete chest recoil ensures that airflow is maximized. As the chest recoils, it creates a negative pressure within the lungs, drawing air in. This negative pressure gradient is essential for optimal ventilation, ensuring that every breath is efficient in delivering oxygen to the bloodstream.
Furthermore, chest recoil facilitates the gas exchange process. As the lungs expand and recoil, the thin-walled alveoli come into close contact with the capillaries that surround them. This close proximity allows for the efficient exchange of oxygen and carbon dioxide, oxygenating the blood and removing waste gases.
In conclusion, chest recoil is a vital physiological mechanism that underpins our very existence. It optimizes airflow, facilitates gas exchange, and enhances lung function, ensuring that every breath we take is a breath of life.
Increased Venous Return: A Vital Role in Enhancing Cardiac Output
The human body is an intricate masterpiece, and its circulatory system plays a fundamental role in sustaining life. Chest recoil, a crucial component of this system, exerts a profound impact on venous return, the process by which blood is transported back to the heart. By enhancing venous return, chest recoil directly contributes to improved cardiac filling and output, ensuring an efficient and uninterrupted flow of oxygenated blood throughout the body.
The Mechanics of Venous Return
Venous return refers to the volume of blood that flows into the heart from the systemic and pulmonary circulations. This process is driven by several factors, including:
- Gravity: Blood in the veins is aided by gravity, which helps it flow downward towards the heart.
- Muscle Pump: Skeletal muscle contractions during activity compress the veins, propelling blood towards the heart.
- Valve System: Veins contain one-way valves that prevent blood from flowing backward.
- Respiratory Pump: Chest recoil plays a crucial role in enhancing venous return.
Chest Recoil and Venous Return
During _inhalation, the diaphragm contracts and the chest cavity expands. This expansion creates *negative pressure* within the chest, which draws blood into the thorax. As a result, the *venous pressure in the chest decreases*, facilitating the flow of blood from the systemic circulation into the right atrium of the heart.
Conversely, during exhalation, the diaphragm relaxes and the chest cavity recoils. This positive pressure within the chest promotes blood flow from the pulmonary circulation into the left atrium of the heart. The alternating expansion and recoil of the chest cavity generate a pumping action that effectively augments venous return.
Improved Cardiac Filling and Output
Increased venous return directly impacts cardiac filling and output. When more blood flows into the heart, the ventricular chambers are better filled, resulting in more forceful contractions. Consequently, the cardiac output, or the volume of blood pumped by the heart per minute, increases.
Benefits of Enhanced Venous Return
Enhanced venous return has numerous benefits for the cardiovascular system, including:
- Improved oxygen delivery to tissues
- Enhanced removal of carbon dioxide from the body
- Increased coronary artery perfusion
- Facilitation of defibrillation and restoration of spontaneous circulation in cardiac arrest
Chest recoil plays a vital role in increasing venous return, thereby improving cardiac filling and output. By enhancing the flow of blood to and from the heart, chest recoil ensures an efficient circulatory system that supports the body’s metabolic demands and overall well-being. Understanding the mechanics and significance of this phenomenon underscores the intricate interconnectedness of our physiological processes.
Chest Recoil: A Lifeline for Optimal Heart Health
In the intricate symphony of our bodies, there exists a remarkable mechanism that plays a pivotal role in sustaining the lifeblood of our hearts – chest recoil. As we inhale, our chests expand, creating a negative pressure that draws air into our lungs. However, it’s the exhalation process that truly unleashes the power of chest recoil.
Upon exhalation, the elastic recoil of our lungs and chest wall springs back into action, passively expelling air from the lungs. This complete chest recoil is critical for maintaining optimal heart health because it:
Enhances Venous Return
The negative pressure generated by chest recoil sucks blood back into the heart. As blood flows from the body’s veins through the superior and inferior vena cavae, the recoil action facilitates efficient venous return. This increased venous return ensures adequate filling of the heart, maximizing the volume of blood available for pumping to the body.
Improves Coronary Artery Perfusion
The heart, like any other organ, requires a steady supply of oxygen to function optimally. Chest recoil plays a crucial role in maintaining coronary blood flow, the lifeline of the heart muscle. As the heart relaxes during the diastolic phase, the recoil of the chest wall creates a negative pressure gradient. This gradient pulls blood into the coronary arteries, delivering vital oxygen to the myocardium, the muscular tissue of the heart.
As the heart contracts, the increased pressure in the chest cavity momentarily reduces coronary blood flow. However, once the heart relaxes, chest recoil quickly restores blood flow to the coronary arteries. This intricate interplay ensures that the heart receives a continuous supply of oxygen, supporting its tireless work of pumping blood throughout the body.
How Chest Recoil Facilitates Efficient Gas Exchange
- Breathing is a vital process that sustains our lives. Every breath we take facilitates the exchange of gases, allowing oxygen to enter our bloodstream and carbon dioxide to be expelled.
- Chest recoil plays a crucial role in this essential process, ensuring the efficient delivery of oxygen to tissues and the removal of waste carbon dioxide.
Expansion of the Lungs
- Chest recoil involves the elastic recoil of the lungs, which act like two balloons that expand and contract with each breath.
- When we inhale, our diaphragm and intercostal muscles contract, pulling the lungs downward and outward, increasing the chest cavity’s volume.
- This expansion creates negative pressure, drawing air into the lungs. As a result, the alveoli, tiny air sacs in the lungs, fill with oxygen-rich air.
Oxygen Delivery to Tissues
- Once the lungs are filled with oxygen, the pulmonary capillaries in the alveoli absorb the oxygen into the bloodstream.
- Hemoglobin, a protein in red blood cells, binds to oxygen, transporting it throughout the body.
- Oxygen-rich blood is then delivered to tissues and cells, where it provides the energy they need to function.
Removal of Carbon Dioxide
- As oxygen is consumed by tissues, carbon dioxide is produced as a waste product.
- Carbon dioxide diffuses back into the bloodstream and is transported to the lungs for elimination.
- In the lungs, carbon dioxide is exhaled through the airways, ensuring that the body maintains a proper balance of gases.
- Chest recoil is an essential mechanism that facilitates the efficient exchange of gases in the lungs.
- It ensures that oxygen is delivered to tissues and carbon dioxide is removed, supporting the body’s vital functions. Without complete chest recoil, gas exchange would be impaired, leading to serious health consequences.
Restoring Spontaneous Circulation: The Vital Role of Chest Recoil
In the face of cardiac arrest, every second counts. Achieving restoration of spontaneous circulation (ROSC) is critical for survival, and chest recoil plays a pivotal role in this life-saving process.
Chest recoil refers to the elastic retraction of the chest wall after compression. This process creates negative pressure within the chest cavity, which facilitates venous return to the heart. The increased venous return enhances cardiac filling and output, delivering oxygenated blood to vital organs and tissues.
Facilitating Defibrillation
Defibrillation, the delivery of a high-energy electrical shock to the heart, aims to restore a normal heart rhythm and stop ventricular fibrillation or pulseless ventricular tachycardia. Chest recoil is essential for successful defibrillation as it improves the contact between the defibrillator pads and the heart. By creating negative pressure within the chest cavity, chest recoil draws the heart closer to the pads, optimizing current flow and increasing the likelihood of successful defibrillation.
Re-establishing Spontaneous Circulation
After successful defibrillation, chest recoil continues to play a crucial role in restoring spontaneous circulation. The increased venous return and improved cardiac output help to establish a self-sustaining heartbeat. The negative pressure generated by chest recoil also assists in dispersing post-shock cardiac arrhythmias and promoting a return to normal electrical activity.
Enhancing Oxygen Delivery
Restoration of spontaneous circulation ensures adequate oxygen delivery to all body tissues. Chest recoil facilitates gas exchange by ensuring complete lung expansion and adequate ventilation. The negative pressure created by chest recoil helps to open up collapsed alveoli and improve airflow, allowing for efficient oxygen uptake and carbon dioxide removal.
By understanding the vital role of chest recoil in achieving ROSC, healthcare providers can optimize their resuscitation efforts in the critical setting of cardiac arrest. Proper execution of chest compressions and defibrillation, in conjunction with appropriate airway management, can enhance chest recoil and significantly improve the chances of survival for patients facing this life-threatening emergency.