The endocrine system plays a crucial role in regulating the excretory system, ensuring electrolyte balance and fluid homeostasis. Key hormones involved include ADH, which regulates water balance, aldosterone, which manages electrolyte balance, and PTH, which influences calcium metabolism. Thyroid hormones also affect metabolic rate and urine output. These hormones work in concert to regulate renal function, impacting water conservation and ion balance. Endocrine system dysfunctions can disrupt renal function, leading to conditions like diabetes insipidus and Cushing’s syndrome. Understanding the endocrine system’s role in excretion is vital for diagnosing and managing renal disorders.
The Endocrine System’s Crucial Role in Renal Function
Introduction:
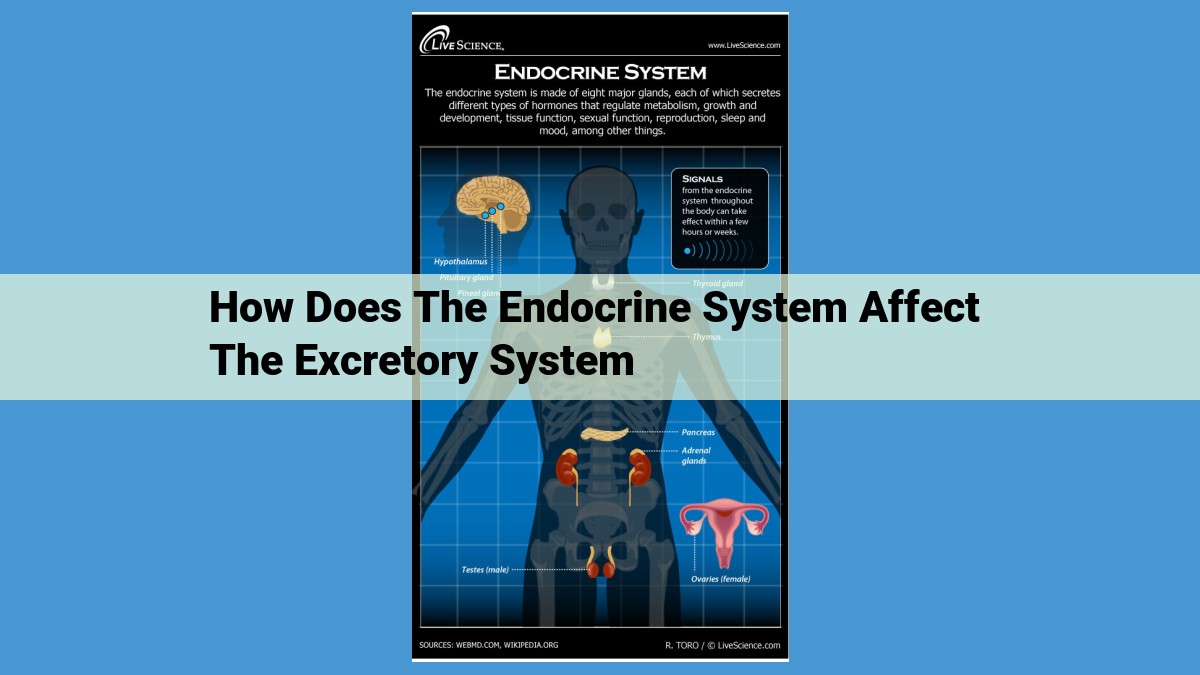
The human body is a complex and interconnected system, where various organs and systems work in concert to maintain optimal function. Among these, the endocrine system and the renal system play a vital role in maintaining fluid and electrolyte balance, ensuring overall health and well-being.
Endocrine System’s Influence on Renal Function:
The endocrine system produces hormones that act as chemical messengers, regulating various bodily functions. Hormones such as antidiuretic hormone (ADH), aldosterone, and parathyroid hormone (PTH) directly impact the kidneys’ ability to excrete salts and water. By controlling the reabsorption and excretion of ions and water, the endocrine system ensures that the body can maintain a stable internal environment.
Key Hormones Involved:
-
Antidiuretic Hormone (ADH): Produced by the pituitary gland, ADH regulates the reabsorption of water in the kidneys. It targets the collecting ducts, increasing their permeability to water, which allows the body to conserve water and reduce urine volume.
-
Aldosterone: Secreted by the adrenal glands, aldosterone regulates sodium and potassium levels in the body. It targets the collecting ducts, increasing sodium reabsorption and potassium secretion, thereby maintaining proper electrolyte balance and blood pressure.
-
Parathyroid Hormone (PTH): Produced by the parathyroid glands, PTH regulates calcium and phosphate metabolism. It influences renal function by reducing phosphate reabsorption and increasing calcium reabsorption in the proximal tubules.
Integration and Impact:
These hormones work in coordination, ensuring that the kidneys can efficiently regulate water and electrolyte balance. ADH helps conserve water, while aldosterone and PTH regulate the excretion of salts and minerals. This integrated hormone action allows the body to maintain a stable internal environment, adapting to changes in fluid intake, electrolyte levels, and blood pressure.
Clinical Implications:
Dysfunctions in the endocrine system can disrupt renal function, leading to various disorders. For example, diabetes insipidus, caused by ADH deficiency, results in excessive water loss and dehydration. Cushing’s syndrome, resulting from excess cortisol production, can cause hypertension and fluid retention due to increased aldosterone levels. Understanding the endocrine system’s role in renal function is crucial for diagnosing and managing such disorders effectively.
Conclusion:
The endocrine system plays an essential role in regulating renal function, ensuring fluid and electrolyte balance in the body. Hormones like ADH, aldosterone, and PTH act on the kidneys to control water and salt excretion, maintaining a stable internal environment. Dysfunctions in the endocrine system can disrupt renal function, highlighting the importance of understanding these interactions for effective diagnosis and management of renal disorders.
Key Hormones Involved in Renal Regulation
The endocrine system plays a crucial role in regulating the kidneys’ excretion of salts and water, ensuring electrolyte balance and fluid homeostasis. Three primary hormones influence renal function: antidiuretic hormone (ADH), aldosterone, and parathyroid hormone (PTH).
ADH (Antidiuretic Hormone)
Produced in the hypothalamus and stored in the pituitary gland, ADH regulates water balance and urine volume. When blood osmolality increases, such as during dehydration, ADH release increases. This ADH then binds to receptors in the kidneys’ collecting ducts, increasing water reabsorption and reducing urine output. ADH helps conserve water, maintaining blood volume and preventing dehydration.
Aldosterone
Secreted by the adrenal glands, aldosterone plays a key role in electrolyte balance and blood pressure regulation. It acts on the kidneys’ collecting ducts, promoting sodium reabsorption and potassium secretion. Increased aldosterone levels, such as in response to low blood volume or high potassium levels, lead to sodium retention and potassium loss. This helps regulate blood pressure by increasing fluid retention and vascular resistance.
PTH (Parathyroid Hormone)
PTH is produced by the parathyroid glands and is responsible for calcium metabolism and urine formation. PTH targets the kidneys’ proximal and distal tubules, promoting calcium reabsorption and phosphate excretion. This process helps maintain calcium homeostasis, essential for bone health and nerve function.
ADH (Antidiuretic Hormone):
In the intricate tapestry of our bodies, the endocrine system plays a masterful role in regulating various processes, including the critical functions of our kidneys. Among these orchestrators, antidiuretic hormone (ADH), also known as vasopressin, stands as a pivotal regulator of water balance and urine volume.
ADH, synthesized in the hypothalamus and stored in the posterior pituitary gland, is released into the bloodstream in response to fluctuations in body fluid osmolality. When the level of solutes in our blood rises, such as during dehydration or excessive salt intake, the hypothalamus detects this increase and triggers ADH release.
The primary target of ADH is the collecting duct of the kidneys, where it exerts its antidiuretic effect. By increasing the permeability of the collecting duct to water, ADH facilitates the reabsorption of water from urine back into the bloodstream. This process effectively concentrates urine, reducing its volume and conserving precious fluids.
Conversely, when blood osmolality decreases, indicating adequate hydration, ADH release is suppressed. The collecting duct becomes less permeable to water, resulting in dilute urine and increased urine volume. This mechanism ensures that the body eliminates excess water while retaining essential solutes.
ADH’s intricate interplay with the kidneys is crucial for maintaining fluid balance and electrolyte homeostasis. Without its regulatory actions, we would either become severely dehydrated or suffer from electrolyte imbalances that could disrupt cellular functions.
Aldosterone: The Master of Electrolyte Balance and Blood Pressure
Introduction:
In the realm of the endocrine system, aldosterone reigns supreme as the master regulator of electrolyte balance and blood pressure. Produced by the adrenal glands, aldosterone orchestrates a symphony of physiological processes that ensure our bodies maintain the delicate equilibrium necessary for optimal health.
Function:
Aldosterone’s primary role is to regulate sodium and potassium levels in the body. It achieves this by acting on the kidneys, where it increases sodium reabsorption and promotes potassium secretion. By controlling sodium levels, aldosterone also influences water retention, ensuring the body’s fluid balance remains stable.
Blood Pressure Regulation:
Aldosterone’s pivotal role extends to blood pressure regulation. By increasing sodium reabsorption, it indirectly increases water retention, which in turn expands blood volume and raises blood pressure. This mechanism ensures that vital organs receive adequate blood flow.
Related Concepts:
Renin-Angiotensin-Aldosterone System (RAAS): Aldosterone is a vital component of the RAAS, a complex hormonal cascade that responds to changes in blood pressure. When blood pressure drops, renin is released, triggering a chain reaction that ultimately leads to aldosterone production.
Electrolyte Imbalances:
Dysfunction in aldosterone production can lead to electrolyte imbalances. Hypoaldosteronism (low aldosterone levels) can cause hyponatremia (low sodium) and hyperkalemia (high potassium). Conversely, hyperaldosteronism (high aldosterone levels) can lead to hypernatremia (high sodium) and hypokalemia (low potassium).
Clinical Implications:
Understanding aldosterone’s role is crucial in diagnosing and treating renal disorders. Cushing’s syndrome, for example, results from excessive aldosterone production and can lead to hypertension (high blood pressure). Conversely, Addison’s disease, caused by insufficient aldosterone, can result in hypotension (low blood pressure) and electrolyte imbalances.
PTH (Parathyroid Hormone): A Regulator of Calcium Metabolism and Urine Formation
Introduction:
The parathyroid hormone (PTH), secreted by the parathyroid glands, is a crucial regulator of calcium metabolism and urine formation. It ensures that the body maintains a healthy balance of calcium and other electrolytes, supporting proper nerve and muscle function.
Source and Function:
PTH is produced when blood calcium levels decrease. It acts on the kidneys, stimulating the reabsorption of calcium from the urine back into the bloodstream. This mechanism helps restore calcium levels to normal.
Related Concepts:
* Vitamin D: PTH enhances the absorption of calcium from the intestines by increasing the activity of vitamin D.
* Bone Metabolism: PTH also promotes the release of calcium from bone into the bloodstream, further contributing to normal calcium levels.
* Phosphate Regulation: PTH inhibits phosphate reabsorption in the kidneys, leading to increased phosphate excretion in the urine.
Impact on Urine Formation:
By influencing calcium reabsorption, PTH affects urine formation. When calcium reabsorption increases, less calcium is excreted in the urine. This results in a decreased urine volume.
Clinical Implications:
Dysfunctions of the endocrine system, including the parathyroid glands, can disrupt renal function. For instance, hyperparathyroidism, a condition of excessive PTH secretion, leads to increased calcium reabsorption in the kidneys, resulting in low urine output and potential kidney stones. Conversely, hypoparathyroidism, where PTH production is deficient, can cause increased urine volume due to reduced calcium reabsorption.
Conclusion:
PTH plays a vital role in maintaining calcium homeostasis and modulating urine formation. Its actions in the kidneys ensure the body’s electrolyte balance and support the proper functioning of various bodily systems. Understanding the endocrine system’s role in excretion, including the influence of PTH, is essential for diagnosing and managing renal disorders effectively.
Thyroid Hormones: Their Impact on Renal Function and Overall Health
Source and Function
Thyroid hormones, produced by the thyroid gland, play a crucial role in regulating the body’s metabolic rate. They significantly influence various physiological processes, including renal function.
Impact on Renal Function
Thyroid hormones enhance the reabsorption of sodium and increase glomerular filtration rate (GFR) in the kidneys. As a result, individuals with hyperthyroidism (excess thyroid hormone) tend to have increased urine output due to the increased GFR, while those with hypothyroidism (deficient thyroid hormone) may experience decreased urine output.
Clinical Implications
Thyroid hormone imbalances can significantly impact renal function. In cases of hyperthyroidism, excessive sodium and water excretion can lead to hyponatremia (low sodium levels) and dehydration. Conversely, hypothyroidism can result in fluid retention and edema (swelling) due to decreased urine output.
Importance of Understanding
Understanding the role of thyroid hormones in renal function is crucial for diagnosing and managing thyroid disorders. Accurate diagnosis helps optimize thyroid hormone levels, ensuring proper renal function and overall health.
Integration and Impact: Orchestrating Renal Function
The endocrine system plays a crucial role in regulating renal function, maintaining the body’s delicate balance of water and electrolytes. Several hormones work together to ensure proper excretion, including antidiuretic hormone (ADH), aldosterone, parathyroid hormone (PTH), and thyroid hormones.
ADH, produced by the hypothalamus, targets the kidneys to regulate water reabsorption. When the body senses a decrease in fluid volume or an increase in blood osmolality, ADH is released. It signals the kidneys to absorb more water, reducing urine output and conserving precious fluids.
Aldosterone, secreted by the adrenal glands, plays a vital role in electrolyte balance. It targets the kidneys to promote sodium reabsorption and potassium secretion. This action helps maintain the proper sodium-potassium ratio in the body. As sodium is reabsorbed, water follows passively, helping to regulate blood pressure and fluid balance.
PTH, released by the parathyroid glands, primarily regulates calcium metabolism. However, it also influences renal function by increasing calcium and phosphate reabsorption from the urine. This helps maintain optimal calcium levels in the blood.
Thyroid hormones, produced by the thyroid gland, also impact renal function. They increase the metabolic rate, which affects urine output. Increased metabolic rate leads to greater water and electrolyte excretion, promoting efficient waste removal.
The interplay of these hormones ensures the coordinated regulation of renal function. ADH conserves water, aldosterone regulates electrolytes, PTH maintains calcium balance, and thyroid hormones impact metabolic rate and water excretion. Together, they fine-tune the body’s internal environment, ensuring efficient waste removal while preserving essential fluids and ions.
Clinical Implications: Endocrine System and Renal Dysfunction
The delicate balance of our excretory system is intricately intertwined with the endocrine system. When dysfunctions arise within this endocrine symphony, the kidneys’ ability to regulate water, electrolytes, and waste excretion can be severely compromised.
Diabetes Insipidus: In this condition, the pituitary gland fails to produce sufficient antidiuretic hormone (ADH). ADH is the gatekeeper of water reabsorption in the kidneys. Without it, the body loses excessive amounts of water through urine, leading to severe dehydration and an inability to concentrate urine.
Cushing’s Syndrome: This condition stems from an overproduction of cortisol by the adrenal glands. Cortisol, known as the “stress hormone,” has a profound effect on water and sodium balance. In Cushing’s syndrome, excessive cortisol suppresses ADH production, resulting in excessive water loss and sodium retention, causing hypertension and other complications.
These examples illustrate how imbalances in the endocrine system can disrupt the kidneys’ ability to regulate fluid and electrolyte homeostasis. Recognizing these clinical implications is crucial for timely diagnosis and effective management of renal disorders. Understanding the intricate interplay between the endocrine system and renal function empowers healthcare professionals to optimize treatment strategies, improve patient outcomes, and prevent further complications.