To calculate TPN, consider the patient’s age, nutritional status, and body composition. Determine the calories needed (carbohydrates, proteins, fats), and calculate the total fluid volume to prevent dehydration or overhydration. Electrolytes, such as sodium and potassium, are crucial for fluid balance and nerve function. Vitamins, classified as water-soluble or fat-soluble, perform essential bodily functions. Trace elements like iron and zinc play vital roles in various processes. Monitor TPN’s effectiveness through laboratory tests and clinical assessments, and adjust its composition as needed to ensure optimal nutrition support.
Total Parenteral Nutrition (TPN): A Lifeline for Nutritional Replenishment
In the realm of healthcare, there are times when individuals encounter situations where their bodies are unable to obtain adequate nutrition through conventional means like eating or drinking. Total Parenteral Nutrition (TPN) emerges as a critical solution in such scenarios, offering a lifeline of essential nutrients directly into the bloodstream.
TPN is a specialized medical intervention that involves administering a carefully formulated solution of nutrients intravenously. This technique provides the body with the necessary building blocks for growth, repair, and optimal functioning. It is typically employed when the digestive system is compromised or non-functional, such as in cases of severe gastrointestinal disorders, major surgeries, or prolonged periods of unconsciousness. By bypassing the digestive tract, TPN ensures that essential nutrients are delivered directly to the bloodstream, ensuring their immediate absorption and utilization by the body.
Basic Principles of TPN: Understanding Its Administration and Limitations
Total parenteral nutrition (TPN) is a life-saving medical intervention that provides essential nutrients directly into the bloodstream when the digestive system is unable to adequately absorb them. TPN involves delivering a customized mixture of nutrients, electrolytes, vitamins, and trace elements through a catheter inserted into a large vein, typically in the chest.
TPN is administered through a continuous infusion pump that delivers the nutrient solution over a 24-hour period. This slow and steady administration allows the body to gradually absorb the nutrients without overwhelming its metabolic processes.
While TPN can provide essential nourishment, it also has certain limitations. It is intended as a temporary solution for individuals who cannot obtain adequate nutrition through oral or enteral feeding methods. It is not a long-term solution and requires close medical supervision to ensure safety and effectiveness.
One of the key challenges with TPN is the risk of infection, as the catheter provides a potential entry point for bacteria into the bloodstream. Strict adherence to sterile techniques and regular monitoring of the catheter site are crucial to prevent infections.
Moreover, TPN can alter the body’s metabolic processes, which can lead to electrolyte imbalances, liver dysfunction, and glucose intolerance. Regular blood tests and close monitoring of the patient’s overall health are essential to adjust the composition of TPN as needed and mitigate any potential complications.
Components of Total Parenteral Nutrition (TPN)
Total Parenteral Nutrition (TPN) is a life-saving medical intervention that provides essential nutrients directly into the veins when the gut cannot absorb them effectively. Understanding the components of TPN is crucial for optimizing its efficacy.
Macronutrients
- Carbohydrates: The primary energy source for the body, carbohydrates are vital for brain function, organ health, and muscle maintenance.
- Proteins: Essential for building and repairing tissues, proteins are crucial for immune function, wound healing, and muscle mass.
- Fats: Providing concentrated energy and supporting cell growth, fats are also vital for hormone production and nerve function.
Electrolytes
Electrolytes are minerals that regulate fluid balance, nerve impulses, and muscle contractions. Key electrolytes in TPN include:
- Sodium: Regulates fluid balance and blood pressure.
- Potassium: Essential for nerve and muscle function.
- Calcium: Supports bone health, nerve function, and muscle contraction.
Vitamins
Vitamins are organic compounds required for various bodily functions. TPN typically includes:
- Water-soluble vitamins: Vitamin C, B vitamins, and niacin, which are essential for metabolic processes and immune function.
- Fat-soluble vitamins: Vitamins A, D, E, and K, which require fat for absorption and support vision, bone health, and blood clotting.
Trace Elements
Trace elements are minerals present in small amounts but essential for specific functions. TPN includes:
- Iron: Essential for red blood cell production.
- Zinc: Supports immune function and wound healing.
- Selenium: Protects cells from damage and supports thyroid function.
By carefully balancing these components, healthcare professionals can customize TPN to meet the individual needs of patients, ensuring they receive the necessary nutrients to support their recovery and well-being.
Calculating the Essential Elements of TPN
The Customized Formula for Nutritional Recovery
Total Parenteral Nutrition (TPN) provides life-sustaining nutrients directly into the bloodstream, bypassing the digestive system. Tailoring the composition of TPN is crucial for each patient’s specific needs.
Factors Influencing Nutrient Requirements
The calculation of TPN’s individual components considers several factors:
- *Age: Different age groups have varying nutritional requirements. Children and the elderly may have different needs compared to adults.
- *Nutritional Assessment: A comprehensive assessment of the patient’s nutritional status provides valuable insights into their current and future requirements.
- *Body Composition: Body composition analysis helps determine the patient’s lean body mass and fat mass, which influences nutrient requirements.
Essential Macronutrients, Electrolytes, Vitamins, and Trace Elements
TPN includes essential macronutrients such as carbohydrates, proteins, and fats, which provide the body with energy and building blocks for tissues. Electrolytes, such as sodium and potassium, regulate fluid balance and nerve function. Vitamins are vital for various bodily processes, while trace elements play crucial roles in metabolism and enzyme function.
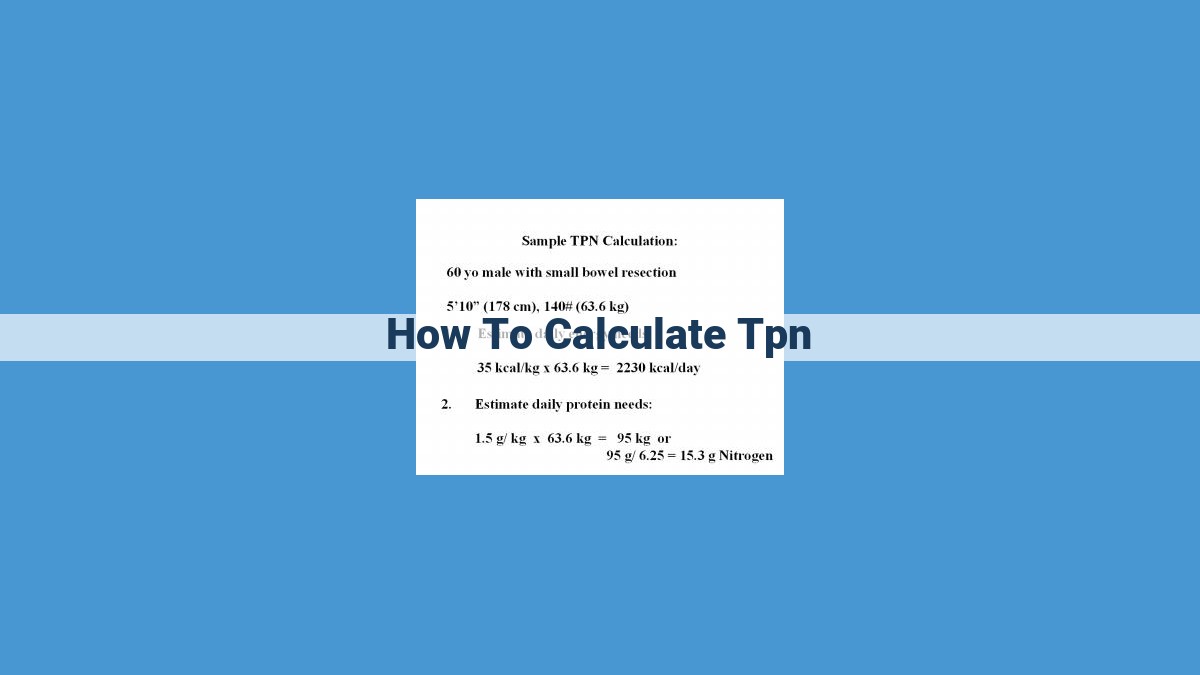
Calculating Nutrient Requirements
The specific composition of TPN is calculated based on the patient’s calorie and protein requirements, as well as their individual electrolyte, vitamin, and trace element needs. These requirements vary depending on factors such as age, activity level, and underlying medical conditions.
Personalized Nutrition for Optimal Outcomes
By considering these factors, healthcare professionals can customize TPN to provide the necessary nutrients for maintaining and restoring the patient’s health. Regular monitoring and adjustments ensure that the composition of TPN remains optimized, delivering the best possible outcomes for the patient.
Calculating the Total Fluid Volume in Total Parenteral Nutrition (TPN): Striking the Delicate Balance
TPN, a highly specialized medical intervention, provides essential nutrients directly into the bloodstream when the digestive system is compromised. Determining the appropriate fluid volume is paramount, as both overhydration and dehydration can lead to serious health complications.
Overhydration: A Pitfall to Avoid
Excessive fluid intake during TPN can place an undue burden on the body’s circulatory system. The heart struggles to pump the extra fluid, potentially leading to congestive heart failure, especially in individuals with pre-existing cardiac conditions. Additionally, overhydration can cause swelling in the legs, hands, and feet.
Dehydration: An Equally Perilous Path
Conversely, inadequate fluid intake during TPN can lead to dehydration. This can manifest as dry mouth, decreased urine output, and constipation. Dehydration can also affect electrolyte balance, impairing nerve function and causing muscle weakness. In extreme cases, dehydration can progress to hypovolemic shock, a life-threatening condition.
Finding the Golden Mean: Individualized Calculations
The appropriate fluid volume in TPN is not a one-size-fits-all equation. It must be tailored to each patient’s unique needs, considering factors such as their age, nutritional status, and body composition.
Age: Infants and children have higher fluid requirements per body weight compared to adults. The younger the patient, the lower the total fluid volume should be, relative to their body size.
Nutritional status: Patients with severe malnutrition may require higher fluid volumes to replen
Electrolytes: Regulating Fluid Balance and Nerve Function in TPN
When delving into the world of Total Parenteral Nutrition (TPN), we can’t overlook the crucial role played by electrolytes. These tiny ions, like sodium and potassium, pack a significant punch in maintaining the delicate balance of our body’s fluids and the proper functioning of our nervous system.
Sodium stands as the most abundant electrolyte in TPN. It’s not just a spectator; sodium actively regulates the distribution of water in our body, ensuring it stays where it’s supposed to. Without enough sodium, we can face dehydration and its unpleasant consequences.
Next up is potassium, another electrolyte that plays a vital role in regulating fluid balance and nerve function. It’s involved in transmitting electrical signals throughout our body, making it indispensable for everything from muscle contractions to the proper rhythm of our heart.
The presence of these electrolytes in TPN is not optional. They’re essential players in maintaining the body’s homeostasis, the delicate balance that keeps us functioning optimally. Without them, dehydration, electrolyte imbalances, and impaired nerve function can rear their ugly heads, potentially leading to severe complications if left unchecked.
Vitamins: Essential Nutrients for Optimal Function
In the realm of Total Parenteral Nutrition (TPN), vitamins play a crucial role in maintaining the body’s vital functions. These organic compounds come in two forms: water-soluble and fat-soluble, each with unique properties and essential roles.
Water-Soluble Vitamins: Facilitating Essential Processes
Water-soluble vitamins, including Vitamin C and B vitamins, are readily absorbed and easily excreted by the body. They serve as coenzymes, substances that assist enzymes in performing important biochemical reactions. For instance, Vitamin C acts as an antioxidant, protecting cells from damaging free radicals, while Vitamin B12 is essential for red blood cell formation and neurological function.
Fat-Soluble Vitamins: Stored for Sustenance
Unlike their water-soluble counterparts, fat-soluble vitamins (Vitamins A, D, E, and K) are absorbed with dietary fat and stored in the body’s fatty tissues. These vitamins play vital roles in various processes. Vitamin A ensures healthy vision and immune function, Vitamin D supports bone health, Vitamin E protects cells from oxidative damage, and Vitamin K is essential for blood clotting.
Ensuring Vitamin Adequacy in TPN
Given their critical roles, it is essential to ensure an adequate supply of vitamins through TPN. Healthcare professionals meticulously calculate the specific composition of TPN solutions based on individual patient requirements, ensuring they receive the necessary amounts of each vitamin. Regular monitoring of vitamin levels through laboratory tests ensures that patients receive the optimal amounts, promoting overall health and well-being.
Trace Elements: Essential Nutrients for Your Body’s Well-being
While trace elements may be present in small amounts in our body, their significance is immeasurable. These micronutrients play crucial roles in various bodily processes, ensuring our optimal health and function.
Iron, for instance, is imperative for red blood cell production, enabling oxygen transport throughout the body. Zinc, on the other hand, is essential for immune function, wound healing, and cell growth. Selenium, though present in trace amounts, is vital for antioxidant defense and thyroid hormone metabolism.
Chromium, a trace element often overlooked, plays a significant role in glucose metabolism, helping to regulate blood sugar levels. Copper is essential for red blood cell formation, nerve function, and connective tissue synthesis. Manganese, involved in bone formation and metabolism, supports healthy bones and joints.
Understanding the critical role of trace elements in our body helps us appreciate the importance of a balanced diet. By consuming a variety of nutrient-rich foods, we can ensure that our bodies have the necessary trace elements to function optimally.
So, next time you think about nutrition, remember not only the macronutrients like carbohydrates, proteins, and fats, but also the indispensable trace elements that underpin our overall well-being.
Monitoring and Adjustment of Total Parenteral Nutrition (TPN)
Ensuring the optimal effectiveness of TPN requires meticulous monitoring and timely adjustments to its composition. This involves a combination of laboratory tests and clinical assessments that provide valuable insights into the patient’s nutritional status and response to TPN.
Laboratory Tests:
Regular blood tests are essential to monitor key parameters that indicate the effectiveness of TPN. These include:
- _Electrolytes (sodium, potassium, chloride): Maintaining electrolyte balance is crucial for fluid regulation and nerve function.
- Glucose: Blood glucose levels are monitored to prevent hyperglycemia or hypoglycemia.
- Triglycerides: Excessive accumulation of triglycerides can indicate metabolic complications.
- Nitrogen balance: This test assesses the body’s protein utilization and helps adjust protein intake.
Clinical Assessments:
In addition to laboratory tests, clinical assessments provide complementary information about the patient’s well-being and nutritional status. These may include:
- Physical examination: This involves assessing the patient’s overall appearance, weight, and hydration status.
- Nutritional assessment: A thorough evaluation of the patient’s nutritional history, dietary intake, and anthropometric measurements.
- Body composition analysis: Techniques such as bioelectrical impedance analysis or dual-energy X-ray absorptiometry can provide insights into body composition and muscle mass.
- Wound assessment: For patients with open wounds, regular inspection and monitoring of wound healing are essential.
Adjustment of TPN:
Based on the results of monitoring, adjustments to the TPN composition may be necessary. This involves modifying the:
- Macronutrient composition: This may include alterations in carbohydrate, protein, or fat intake based on energy needs and nutritional status.
- Electrolyte balance: Electrolyte levels must be closely monitored and adjusted to prevent imbalances.
- Vitamin and mineral supplementation: Vitamin and mineral levels are re-evaluated and adjusted as needed to ensure adequate intake.
- Fluid volume: The total fluid volume may be adjusted based on the patient’s fluid status and tolerance.
Importance of Monitoring and Adjustment:
Regular monitoring and adjustment of TPN are crucial for:
- Preventing complications: By identifying and addressing any deficiencies or imbalances early on, complications such as infection, electrolyte imbalances, or metabolic disturbances can be avoided.
- Optimizing nutritional status: Tailoring TPN to the patient’s individual needs ensures they receive the necessary nutrients for optimal healing and recovery.
- Improving patient outcomes: Effective monitoring and adjustment contribute to improved patient outcomes, reduced hospital stays, and enhanced overall well-being.