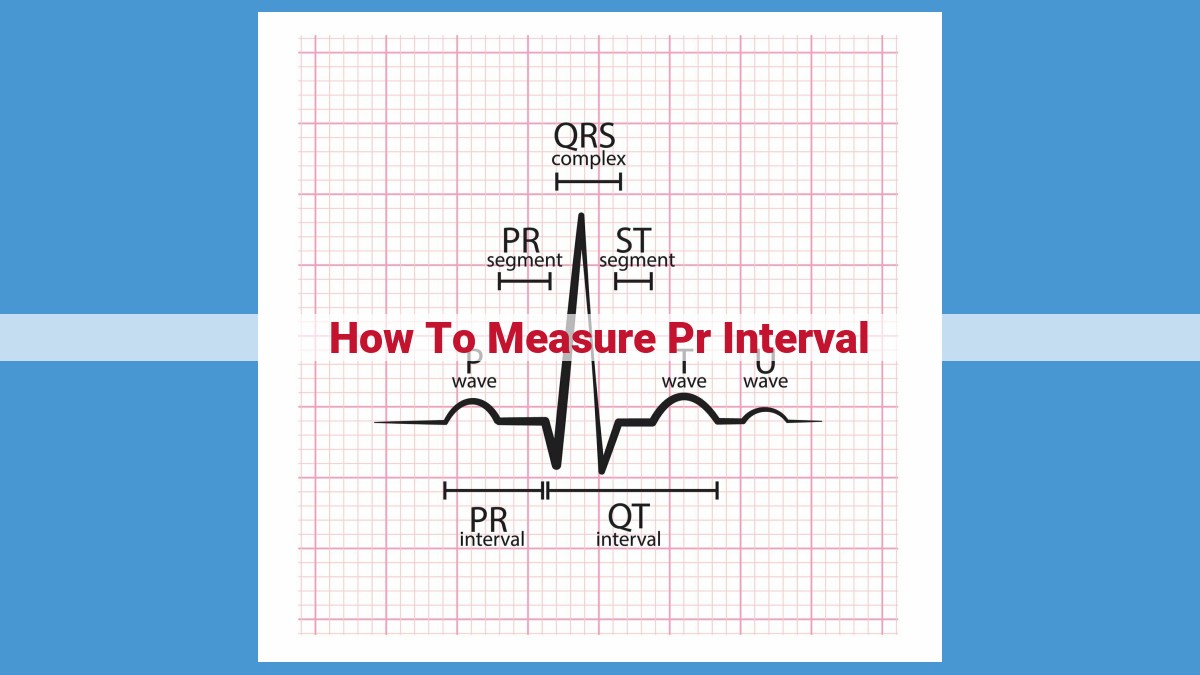
To measure the PR interval, locate the P wave, which represents atrial depolarization, and QRS complex, which signifies ventricular depolarization, on an electrocardiogram (ECG). Measure the time between the start of the P wave to the start of the QRS complex using a ruler or calipers. The normal PR interval duration ranges from 120 to 200 milliseconds. Prolonged PR intervals may indicate conduction delays within the heart’s electrical system, while shortened PR intervals can suggest abnormal pathways.
- Importance of studying the PR interval
- Review of the anatomy and physiology of the heart’s electrical conduction system
Understanding the Heart’s Electrical System: The Importance of the PR Interval
The human heart is an extraordinary organ that pumps blood throughout our bodies, providing vital oxygen and nutrients to our cells. At the core of its functionality lies an intricate electrical system that orchestrates the heart’s rhythmic contractions. Understanding this electrical system is paramount for diagnosing and treating various cardiovascular conditions. Among the crucial components of this system is the PR interval, which provides insight into the heart’s conduction pathways and potential abnormalities.
Anatomy and Physiology of the Heart’s Electrical Conduction System
The heart’s electrical system consists of specialized cells called pacemaker cells that generate electrical impulses. These impulses travel through the heart via specialized pathways, initiating the coordinated contraction of the heart’s chambers. The electrical impulses originate in the sinoatrial node (SA node), located in the right atrium. The SA node acts as the heart’s natural pacemaker, setting the pace for the electrical impulses.
From the SA node, the electrical impulses travel through the atrial pathways, causing the atria (the heart’s upper chambers) to contract. The impulses then reach the atrioventricular node (AV node), a crucial checkpoint that delays the electrical signals before they reach the ventricles (the heart’s lower chambers). This delay, known as the PR interval, allows the atria to fill with blood before the ventricles contract.
The PR Interval: Significance and Factors Affecting Its Duration
The PR interval is a measurement of the time it takes for the electrical impulse to travel from the beginning of the P wave (representing atrial depolarization) to the beginning of the QRS complex (representing ventricular depolarization). This interval provides valuable information about the conduction properties of the AV node and the overall integrity of the heart’s electrical system.
The normal PR interval ranges from 0.12 to 0.20 seconds. Prolonged PR intervals (greater than 0.20 seconds) may indicate a conduction delay within the AV node, a condition known as atrioventricular block. Conversely, shortened PR intervals (less than 0.12 seconds) can suggest an abnormally fast conduction pathway, such as in Wolff-Parkinson-White syndrome.
Factors such as age, heart rate, and medications can influence the PR interval. For instance, the PR interval tends to increase with age due to the gradual slowing of the AV node conduction. Elevated heart rates can also shorten the PR interval, as the faster the heart beats, the less time the electrical impulse spends in the AV node.
The P Wave: A Tale of Atrial Depolarization
In the symphony of our heartbeat, the P wave plays a crucial role, setting the stage for the powerful contractions that pump life-giving blood throughout our bodies. This tiny electrical impulse marks the beginning of the heart’s electrical journey, initiating the coordinated dance of the heart’s chambers.
Genesis of the P Wave
The sinoatrial node (SA node), the heart’s natural pacemaker, generates the P wave. Located in the right atrium, the SA node acts as an electrical conductor, initiating the depolarization process that triggers atrial muscle contraction.
Unveiling Atrial Depolarization
Depolarization is the process of electrical excitation that spreads across the heart’s cells. When the SA node sends out its electrical signal, the P wave represents the initial depolarization of the atria, the heart’s upper chambers. This electrical wavefront sweeps across the atrial walls, causing the atria to contract and pump blood into the ventricles, the heart’s lower chambers.
The P Wave and PR Interval: A Tale of Two Intervals
The PR interval, the time between the onset of the P wave and the beginning of the QRS complex, provides valuable insights into the heart’s electrical conduction system. It represents the delay in electrical signals traveling through the atrioventricular node (AV node), the gatekeeper between the atria and ventricles. A normal PR interval signifies proper conduction through the AV node, while abnormalities can indicate potential heart conditions.
Understanding the P wave and its relationship to the PR interval is essential for unraveling the intricacies of the heart’s electrical system. By identifying and interpreting these electrical impulses, healthcare professionals can assess the heart’s health and diagnose conditions that may affect its rhythm and efficiency.
The PR Interval: Understanding the Heart’s Electrical Conduction
The human heart, a tireless pump, relies on an intricate web of electrical signals to orchestrate its rhythmic contractions. Measuring these signals through an electrocardiogram (ECG) unveils valuable insights into the heart’s inner workings. One crucial parameter is the PR interval, a window into the heart’s conduction system that ensures coordinated atrial and ventricular contractions.
Defining the PR Interval
The PR interval, measured in milliseconds, represents the time elapsed between the start of atrial depolarization, recorded as the P wave, and the onset of ventricular depolarization, seen as the QRS complex. It reflects the conduction delay within the atrioventricular node (AV node), a specialized structure that acts as a gatekeeper, slowing down the electrical impulses to allow for ventricular filling.
The Significance of the PR Interval
Optimal PR interval duration is essential for the heart’s efficient pumping function. A prolonged PR interval can indicate delays in electrical conduction through the AV node, which may compromise ventricular filling and lead to conditions such as heart block. Conversely, a shortened PR interval may suggest faster-than-normal conduction, potentially associated with atrial fibrillation or premature ventricular contractions.
Factors Influencing the PR Interval
Various factors can influence the duration of the PR interval, including:
- Age: The PR interval tends to lengthen with age.
- Exercise: Exercise can temporarily shorten the PR interval.
- Electrolyte abnormalities: High potassium or low calcium levels can prolong the PR interval.
- Medications: Certain drugs, such as beta-blockers, can prolong the PR interval.
Understanding the Electrocardiogram (ECG)
An ECG is a valuable tool for assessing the heart’s electrical activity. Its characteristic deflections, including the P wave, PR interval, QRS complex, and T wave, provide a visual representation of the heart’s electrical impulses. Skilled interpreters can analyze these deflections to identify normal and abnormal patterns, aiding in the diagnosis and management of cardiovascular conditions.
The PR interval serves as a vital indicator of the heart’s electrical conduction. Its measurement is crucial for assessing the heart’s ability to coordinate atrial and ventricular contractions. Electrocardiography remains the cornerstone of cardiac monitoring, enabling healthcare professionals to detect and treat cardiovascular disorders effectively, ensuring that the heart continues its tireless dance of life.
The QRS Complex: Unveiling Ventricular Depolarization
In the realm of the heart’s electrical symphony, the QRS complex stands as a captivating crescendo, heralding the crucial moment of ventricular depolarization. This vital process sets the stage for the forceful contraction of the heart’s ventricles, the muscular chambers responsible for pumping blood throughout our bodies.
Defining the QRS Complex: A Snapshot of Ventricular Excitation
The QRS complex is a distinctive waveform on an electrocardiogram (ECG) that captures the rapid depolarization, or electrical activation, of the ventricles. It typically consists of three deflections: the Q wave, R wave, and S wave.
Ventricular Depolarization: A Journey of Electrical Impulse
Ventricular depolarization is a precisely choreographed cascade of events. It begins with an electrical impulse from the heart’s atrioventricular (AV) node, which triggers the coordinated contraction of the muscular walls of the ventricles.
As the impulse spreads through the ventricles, it depolarizes their cells, causing them to contract and generate the pumping force necessary for circulation. This process is reflected in the QRS complex’s waveform as the Q, R, and S waves represent different stages of ventricular depolarization.
Relationship with the T Wave: A Tale of Two Polarizations
The QRS complex is closely intertwined with the T wave on the ECG. The T wave represents ventricular repolarization, the process by which the ventricles recover and prepare for the next electrical impulse.
The relationship between the QRS complex and the T wave is crucial for understanding the heart’s electrical cycle. Proper repolarization ensures that the ventricles are ready to contract again, preventing arrhythmias and maintaining a healthy heartbeat.
Significance of the QRS Complex: A Diagnostic Lifeline
Measuring the QRS complex is an invaluable tool in diagnosing and managing cardiovascular conditions. Abnormalities in its duration, shape, or presence can point to underlying issues, such as:
- Delayed ventricular depolarization (prolonged PR interval)
- Ventricular hypertrophy (increased QRS amplitude)
- Bundle branch block (altered QRS pattern)
Understanding the QRS complex and its role in ventricular depolarization empowers us to delve into the intricate workings of the heart. Through ECG monitoring, we can uncover hidden cardiovascular disorders and pave the way for effective treatments, ensuring the harmonious beating of our vital organ.
The T Wave: Ventricular Repolarization
After the QRS complex signifies the heart’s ventricles contracting, the T wave plays a crucial role in the relaxation phase. It represents the process of ventricular repolarization, where the electrical impulses are reversed, allowing the ventricles to return to their resting state.
Process of Ventricular Repolarization
The T wave signifies the restoration of the ventricles’ electrical balance. This begins when positively charged ions (sodium and calcium) that rushed into the cells during depolarization start exiting, while negatively charged ions (potassium) flow in. As the cells regain their resting membrane potential, the positive charge diminishes, resulting in the formation of the T wave on the electrocardiogram (ECG).
Relationship with the QRS Complex
The T wave is a subtle deflection that follows the QRS complex. Its shape and direction provide valuable insights into the heart’s electrical activity. Normally, the T wave has an upright appearance and is opposite in polarity to the preceding QRS complex. This indicates normal ventricular repolarization.
Importance of the T Wave
The T wave serves as a diagnostic tool for various cardiac conditions. Abnormalities in the T wave’s morphology, amplitude, or duration can indicate:
- Ischemia: Decreased blood flow to the heart
- Electrolyte imbalances: Particularly potassium and calcium abnormalities
- Arrhythmias: Irregular heart rhythms
- Other heart conditions: Such as pericarditis, myocarditis, and cardiomyopathy
The T wave is an integral part of the ECG, representing ventricular repolarization. By understanding its significance and relationship with the QRS complex, healthcare professionals can gain valuable insights into the heart’s electrical function and diagnose various cardiac conditions.
The Electrocardiogram (ECG): Capturing the Heart’s Electrical Symphony
Imagine your heart as an orchestra, where each beat is a harmonious melody. The electrocardiogram (ECG) is like a conductor, recording this symphony of electrical impulses that govern your heart’s activity. Join us on a journey to decipher this musical masterpiece and unveil the secrets of the heart’s electrical system.
How an ECG Records Heart Activity
An ECG is a noninvasive test that measures the electrical activity of your heart using electrodes placed on your skin. These electrodes capture the tiny electrical signals generated by your heart’s electrical system, allowing us to visualize the heart’s rhythm and identify any abnormalities.
ECG Deflections: A Musical Score
The ECG displays a series of deflections that represent different phases of your heart’s electrical cycle. These include:
- P wave: Depolarization (electrical activation) of the atria (upper chambers of the heart)
- PR interval: Time delay between atrial and ventricular depolarization (atrioventricular conduction delay)
- QRS complex: Depolarization of the ventricles (lower chambers of the heart)
- T wave: Repolarization (electrical recovery) of the ventricles
Accurate ECG Interpretation: The Key to Clarity
To interpret an ECG accurately, standard recording speeds and calibration marks are crucial. These ensure that the time and amplitude of the deflections are accurately captured, enabling precise diagnosis of any potential heart conditions.
The ECG plays an invaluable role in diagnosing and managing cardiovascular conditions. It helps identify disorders of rhythm (arrhythmias), conduction delays, and myocardial infarction (heart attacks). By capturing the heart’s electrical symphony, the ECG empowers healthcare professionals to unravel its secrets and optimize your heart’s health.