Tidal volume, the volume of air inhaled or exhaled per breath, is a crucial lung function parameter. Spirometry, a standard measurement tool, estimates tidal volume by capturing airflow changes. Pneumotachography directly measures airflow, contributing to tidal volume calculations. Whole-body plethysmography provides a comprehensive assessment, including tidal volume. Additionally, the esophageal balloon technique measures esophageal pressure, which correlates with tidal volume. Understanding these measurement techniques empowers healthcare providers to accurately assess lung function and diagnose respiratory conditions.
Understanding Tidal Volume: A Vital Lung Function
Tidal volume, the amount of air that flows in and out of your lungs during normal breathing, is a crucial aspect of lung function. It helps maintain adequate levels of oxygen in the blood and eliminate carbon dioxide. Measuring tidal volume accurately is essential for evaluating respiratory health, and various techniques exist to do so.
Spirometry: The Standard Measurement
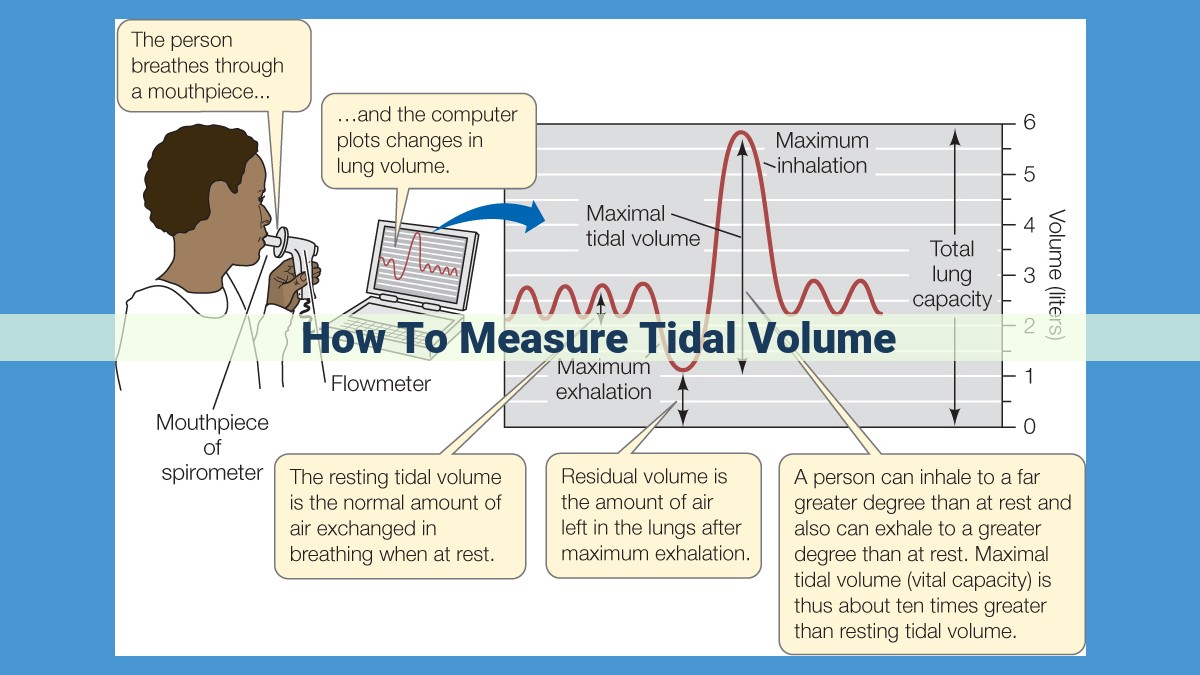
Spirometry is a widely used technique for measuring tidal volume. It involves breathing into a mouthpiece connected to a machine that records the volume and airflow over time. This simple and non-invasive test provides valuable insights into lung function, including vital capacity, forced expiratory volume, and tidal volume.
Pneumotachography: Measuring Airflow
Pneumotachography is another technique that measures airflow, which is key to calculating tidal volume. A pneumotachograph, a device that measures the resistance to airflow, is placed in the mouthpiece or airway. By measuring the pressure drop across the device, airflow can be determined. Combined with other measurements, such as lung volume and chest wall movement, tidal volume can be accurately calculated.
Whole-Body Plethysmography: Comprehensive Assessment
Whole-body plethysmography is a technique that assesses lung function by measuring changes in body volume. The patient is seated in an airtight chamber, and the pressure changes within the chamber are recorded. These changes in pressure correspond to changes in lung volume, including tidal volume. Whole-body plethysmography provides a comprehensive analysis of lung function and can detect even small abnormalities.
Esophageal Balloon Technique: Measuring Esophageal Pressure
The esophageal balloon technique involves inserting a small balloon into the esophagus. By measuring the pressure within the balloon, changes in lung volume can be inferred. This technique is particularly useful in patients who are unable to perform spirometry or when more precise measurements of tidal volume are required.
Importance of Tidal Volume Measurement
Measuring tidal volume accurately is crucial for diagnosing and managing various respiratory conditions. It can help identify issues such as restrictive lung diseases, obstructive lung diseases, and respiratory muscle weakness. Regular monitoring of tidal volume is also important for patients with chronic respiratory diseases, such as asthma and chronic obstructive pulmonary disease (COPD), to assess the effectiveness of treatment and monitor disease progression.
Spirometry: The Gold Standard for Measuring Tidal Volume
Tidal volume, the volume of air that moves in and out of your lungs with each breath, is a crucial indicator of your respiratory health. Assessing tidal volume accurately is essential for diagnosing and managing respiratory conditions. Spirometry, a pulmonary function test, is the most widely used method for measuring tidal volume and other lung function parameters.
Spirometry involves blowing into a mouthpiece connected to a spirometer, which records airflow and volume. As you breathe in and out, the spirometer measures the amount of air you inhale and exhale, as well as the volume of air in your lungs at different points in the respiratory cycle.
Parameters Measured by Spirometry:
- Tidal volume (TV): The volume of air inhaled or exhaled in a single breath.
- Forced vital capacity (FVC): The maximum volume of air you can forcibly exhale after a full inhalation.
- Forced expiratory volume in one second (FEV1): The volume of air you can forcibly exhale in the first second of the FVC maneuver.
- Peak expiratory flow (PEF): The maximum rate of airflow during the FVC maneuver.
Tidal volume is a critical parameter in evaluating lung function. Low tidal volume can indicate respiratory muscle weakness or airway obstruction, while high tidal volume may suggest hyperventilation or overinflation of the lungs.
Spirometry is a non-invasive and relatively simple procedure that can provide valuable insights into your lung health. By accurately measuring tidal volume and other lung function parameters, spirometry helps diagnose and monitor conditions such as asthma, chronic obstructive pulmonary disease (COPD), and cystic fibrosis.
Pneumotachography: The Breathtaking Tool for Measuring Airflow
In the realm of respiratory mechanics, pneumotachography stands tall as a crucial technique for measuring airflow. This non-invasive method plays a pivotal role in determining tidal volume, the fundamental measure of lung function.
How Pneumotachography Works
Pneumotachography harnesses a deceptively simple principle—measuring pressure drop across a resistor. As air flows through a narrow tube with a known resistance, it encounters friction, causing a pressure difference across the tube. Specialized sensors capture this pressure drop, which is proportional to the airflow rate.
Its Role in Tidal Volume Calculation
Tidal volume represents the amount of air inhaled or exhaled with each breath. To calculate tidal volume using pneumotachography, the following formula is employed:
Tidal Volume = Flow Rate × Breath Duration
Pneumotachography measures airflow rate, while spirometry or other methods determine breath duration. By combining these measurements, we can accurately quantify tidal volume.
Benefits of Pneumotachography
Pneumotachography offers several advantages over other methods:
- Non-invasive: It does not require invasive procedures like esophageal balloons or tracheal intubation.
- Continuous: It provides real-time airflow data, allowing for detailed analysis of breathing patterns.
- Versatile: It can be used in a variety of settings, including clinical, research, and occupational health.
Pneumotachography is an indispensable tool for measuring airflow, which is essential for calculating tidal volume. Its non-invasive nature, continuous measurement capabilities, and versatility make it a widely used and trusted technique in the field of respiratory mechanics. By understanding pneumotachography’s role, we gain valuable insights into the intricate workings of our lungs.
Whole-Body Plethysmography: A Comprehensive Lung Function Assessment
Dive into the world of lung function evaluation with a detailed exploration of whole-body plethysmography. This remarkable technique empowers healthcare professionals to unveil a wealth of insights into your respiratory health.
Unlike spirometry, which focuses solely on measuring airflow, whole-body plethysmography takes a comprehensive approach. It encapsulates the entire body within an airtight chamber and measures changes in pressure within the lungs. This ingenious setup enables the precise determination of tidal volume, the volume of air inhaled and exhaled with each breath.
Beyond tidal volume, whole-body plethysmography also provides crucial information about airway resistance, lung compliance, and total lung capacity. These parameters offer a more holistic understanding of lung function, helping diagnose various respiratory conditions, including asthma, chronic obstructive pulmonary disease (COPD), and restrictive lung diseases.
Step into the realm of whole-body plethysmography and unravel the intricacies of your respiratory system. This non-invasive and highly informative technique serves as a cornerstone in diagnosing and managing pulmonary disorders, paving the path to optimal lung health.
Esophageal Balloon Technique: Measuring Esophageal Pressure for Tidal Volume Calculations
Understanding your lung function is crucial for overall health and well-being. Tidal volume plays a vital role in this assessment, and the esophageal balloon technique is a specialized method used to measure it.
The Esophageal Balloon Technique
This technique involves placing a thin balloon into the esophagus, the tube that carries food from the mouth to the stomach. Once inserted, the balloon is inflated, creating a seal that allows for the measurement of esophageal pressure. This pressure reflects the pressure changes within the chest cavity, which are directly related to the expansion and contraction of the lungs.
Measuring Airflow and Esophageal Pressure
By simultaneously measuring airflow using a pneumotachograph and esophageal pressure using the balloon, healthcare professionals can accurately calculate tidal volume. As you inhale, the lungs expand, reducing esophageal pressure. Exhalation causes the lungs to recoil, increasing esophageal pressure. These pressure changes are recorded and analyzed to determine the volume of air moved in and out of the lungs.
Significance for Tidal Volume Calculations
The esophageal balloon technique provides an indirect measurement of tidal volume, as it relies on the assumption that esophageal pressure changes directly reflect lung volume changes. This method is considered reliable and can be used in various settings, including research, clinical practice, and pulmonary function testing.
Additional Benefits
In addition to measuring tidal volume, the esophageal balloon technique can also provide information about:
- Airway resistance: Resistance encountered by air as it flows through the airways.
- Elastic properties of the lungs: The stiffness of the lung tissue.
- Diaphragmatic function: The strength and coordination of the diaphragm, the primary muscle responsible for breathing.
By combining these measurements, healthcare professionals can gain a comprehensive understanding of your lung function and diagnose various respiratory conditions.