The optimal frequency of TPN tubing changes depends on several factors, including the type of tubing used, TPN solution, additives, and patient characteristics. To determine the right frequency, healthcare professionals consider the stability of the TPN solution, potential interactions between additives and tubing materials, and the patient’s age, health status, and underlying conditions. Additive compatibility and patient factors can influence the frequency, as improper changes can lead to complications such as infection or malnutrition. Proper handling and maintenance of TPN tubing are crucial to extend its lifespan and minimize changes. Adhering to the recommended frequency of tubing changes ensures the safety and effectiveness of TPN therapy.
Types of TPN Tubing: Essential Considerations for Optimal Healthcare
When it comes to Total Parenteral Nutrition (TPN), the type of tubing used plays a crucial role in ensuring patient safety and treatment effectiveness. Understanding the different types of TPN tubing and their respective characteristics is essential for healthcare professionals to provide optimal care.
TPN tubing serves as the lifeline that delivers essential nutrients directly into the bloodstream. It is typically made from either PVC (polyvinyl chloride) or silicone. Each material offers distinct advantages and drawbacks:
PVC-based Tubing
- Advantages:
- Relatively inexpensive
- Durable and resistant to kinking
- Disadvantages:
- Contains phthalates, which can leach into the TPN solution
- Less flexible, which can make insertion and removal more challenging
Silicone-based Tubing
- Advantages:
- Phthalate-free, reducing the risk of contamination
- More flexible, allowing for easier insertion and removal
- Disadvantages:
- More expensive than PVC-based tubing
- Prone to tearing or puncturing
The choice between PVC-based and silicone-based tubing depends on the specific patient’s needs and the healthcare provider’s preferences. Factors such as patient age, underlying health conditions, and the duration of TPN therapy should be considered when making this decision.
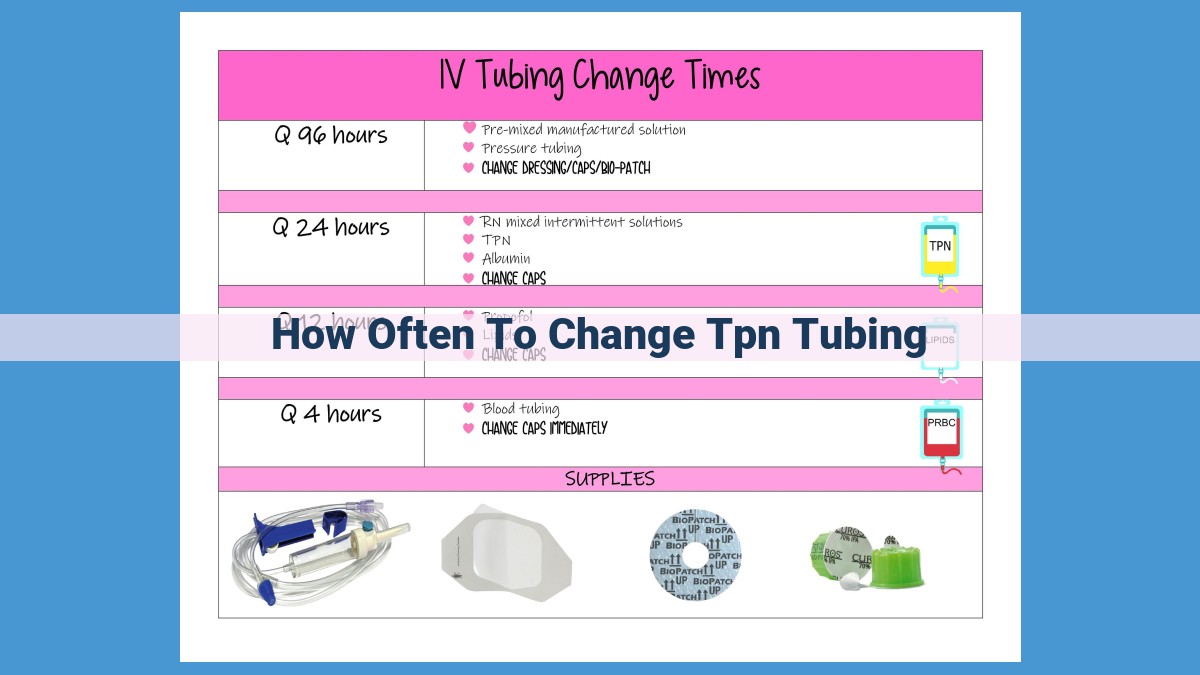
Frequency of TPN Tubing Changes: Factors to Consider
Total parenteral nutrition (TPN) is a life-sustaining therapy that provides essential nutrients directly into the bloodstream. Tubing is a critical component of TPN, carrying the nutrient solution from the bag to the patient’s body. Determining the optimal frequency of TPN tubing changes is crucial for ensuring the safety and effectiveness of this therapy.
Factors Influencing Tubing Change Frequency
Several factors influence how often TPN tubing should be changed, including:
- Type of Tubing: PVC-based tubing has a shorter lifespan compared to silicone-based tubing.
- TPN Solution: The type of TPN solution (formulation and osmolality) can affect the degradation rate of the tubing.
- Additives: Certain additives, such as lipids and vitamins, can degrade the tubing faster.
- Patient Factors: Age, health status, and underlying conditions (e.g., diabetes) may impact the frequency of tubing changes.
Determining the Right Frequency
Healthcare professionals can determine the optimal frequency of tubing changes based on the following considerations:
- Assessment of Tubing Integrity: Inspecting tubing for signs of damage, discoloration, or clogging.
- TPN Solution Stability: Monitoring the solution for stability and potential interactions with the tubing.
- Patient Monitoring: Assessing patient tolerance and response to TPN therapy, including signs of infection or malnutrition.
Additive Considerations
Additives play a significant role in determining tubing change frequency. Lipids, for example, can degrade PVC-based tubing more rapidly. Emulsified lipids have a slower degradation effect, but they still require more frequent tubing changes compared to non-lipid solutions.
Patient Factors
Patient factors also influence the frequency of tubing changes. Younger patients or those with severe underlying conditions may require more frequent changes due to increased metabolic rates or higher risk of infection.
Consequences of Incorrect Frequency
Changing tubing too frequently can lead to unnecessary waste and inconvenience. Conversely, changing it infrequently can increase the risk of complications such as:
- Infection: Old tubing can harbor bacteria, leading to bloodstream infections.
- Malnutrition: Compromised tubing integrity can prevent adequate nutrient delivery.
- Catheter Issues: Damaged tubing can cause problems with catheter function.
Determining the optimal frequency of TPN tubing changes is essential for the safe and effective administration of this therapy. Healthcare professionals must consider various factors, including tubing type, TPN solution, additives, and patient characteristics. By adhering to the recommended frequency, they can ensure the continuous delivery of essential nutrients and minimize the risk of complications.
Determining the Optimal Frequency of TPN Tubing Changes
When it comes to TPN therapy, the frequency of tubing changes is crucial for maintaining patient safety and the efficacy of the treatment. Healthcare professionals play a vital role in determining the optimal frequency based on the unique needs of each patient and their TPN regimen. Here’s a step-by-step guide to help healthcare providers navigate this critical decision.
1. Consider Tubing Type and TPN Solution:
The type of tubing used in TPN therapy and the TPN solution’s composition can influence the frequency of changes. For instance, PVC-based tubing is more prone to lipid absorption, requiring more frequent changes than silicone-based tubing. Similarly, TPN solutions with higher lipid content may necessitate more frequent tubing changes to prevent lipid deposition.
2. Assess Patient Factors:
Patient factors, such as age, health status, and underlying conditions, can impact the frequency of tubing changes. Younger patients with compromised immune systems or infectious complications may require more frequent changes to minimize the risk of infections. Conversely, stable patients with good overall health may be able to tolerate longer intervals between changes.
3. Evaluate Additive Usage:
Additives in TPN solutions, such as vitamins or medications, can affect tubing integrity and the frequency of changes. Some additives can interact with tubing materials, potentially causing degradation or leaching of harmful substances. Healthcare providers must consider the type of additives being used and their potential impact on tubing lifespan.
4. Monitor Clinical Parameters:
Regularly monitoring clinical parameters, such as patient weight, fluid balance, and laboratory values, can provide valuable insights into the adequacy of TPN therapy and the need for tubing changes. If a patient shows signs of malnutrition, fluid overload, or catheter-related complications, more frequent tubing changes may be warranted.
5. Review Manufacturer’s Guidelines and Consult Experts:
Manufacturers of TPN tubing and TPN solutions typically provide guidelines on the recommended frequency of changes. Healthcare professionals should carefully follow these instructions and consult with experienced clinicians or pharmacists when necessary to determine the most appropriate frequency for their patients.
By following these steps, healthcare professionals can determine the optimal frequency of TPN tubing changes, ensuring the safety and effectiveness of TPN therapy while minimizing the risks of complications and maximizing patient outcomes. It’s essential to remember that the frequency of changes is not a fixed number but rather a decision that requires individualized assessment and ongoing monitoring.
Additive Considerations in TPN Tubing
Additives play a crucial role in TPN therapy by providing essential nutrients or medications tailored to each patient’s specific needs. However, these additives can have a significant impact on the integrity of TPN tubing.
Lipid emulsions, a common additive in TPN, can degrade the tubing material, making it more prone to cracking or leaking. This is particularly concerning with PVC-based tubing, which is more susceptible to lipid damage than silicone-based tubing.
Electrolytes and vitamins can also affect tubing integrity. High concentrations of electrolytes can lead to precipitation, forming crystals that can clog the tubing. Similarly, some vitamins, such as vitamin C, can oxidize the tubing material, weakening it over time.
The presence of medications in TPN can further complicate the situation. Certain medications can interact with the tubing material or alter its permeability, potentially compromising the delivery of nutrients.
Therefore, it is crucial to consider the type and concentration of additives when determining the frequency of TPN tubing changes. The healthcare team should assess the compatibility of additives with the tubing material and adjust the replacement schedule accordingly. By carefully managing additive considerations, healthcare professionals can ensure the safe and effective delivery of TPN therapy.
Patient Factors Influencing TPN Tubing Change Frequency
The frequency of TPN tubing changes is not a one-size-fits-all approach. Several patient-specific factors play a crucial role in determining the optimal interval.
Age:
- Younger patients: May require more frequent changes due to their higher metabolic rates and increased fluid needs. Their delicate immune systems are also more vulnerable to infections, making timely tubing changes essential.
Health Status:
- Critically ill patients: Often have compromised immune systems and may need increased tubing changes to prevent infections.
- Diabetic patients: May experience hyperglycemia if TPN solution leaks from damaged or contaminated tubing. Closer monitoring and more frequent changes are necessary.
Underlying Conditions:
- Hepatic disease: Impairs the body’s ability to metabolize certain nutrients, leading to a buildup of toxins in the blood. More frequent tubing changes help remove these toxins and prevent complications.
- Renal disease: Affects fluid balance and electrolyte levels. Tubing changes are crucial to maintain appropriate fluid and electrolyte levels, preventing dehydration or electrolyte imbalances.
Understanding the unique needs of each patient is essential for healthcare professionals to determine an individualized frequency of TPN tubing changes. By considering these patient-specific factors, they can ensure that patients receive optimal care while minimizing the risk of complications.
Consequences of Incorrect Frequency of TPN Tubing Changes
The frequency of TPN tubing changes is crucial for the safety and efficacy of TPN therapy. Incorrect frequency can lead to various complications that can compromise the patient’s well-being.
Too Frequent Changes:
Changing TPN tubing more often than necessary can increase the risk of infection. Every time the tubing is disconnected and reconnected, there’s a chance for bacteria to enter the system. Additionally, excessive handling can damage the tubing and introduce contaminants.
Infrequent Changes:
On the other hand, changing tubing infrequently can lead to malnutrition as the tubing becomes obstructed by precipitates and biofilm formation. Clogged tubing can prevent adequate nutrient delivery, resulting in nutritional deficiencies.
Furthermore, infrequent tubing changes increase the risk of catheter issues. Prolonged use of contaminated tubing can lead to catheter blockage, infection, and even catheter failure.
Balance is Key:
Determining the optimal frequency of tubing changes requires careful consideration of the patient’s individual needs and TPN regimen. Healthcare professionals must strike a balance between minimizing the risk of infection and ensuring adequate nutrient delivery.
Ignorance of these consequences can have severe repercussions on the patient’s health and well-being. Adhering to proper guidelines and monitoring tubing condition is essential to prevent complications and maintain the effectiveness of TPN therapy.
Proper Handling and Maintenance of TPN Tubing for Extended Longevity
In the realm of Total Parenteral Nutrition (TPN), the integrity and longevity of the tubing play a crucial role in ensuring the safety and effectiveness of therapy. Proper handling and maintenance techniques are essential to extend the lifespan of TPN tubing, minimizing the frequency of costly and potentially disruptive changes.
Handling with Care
From the outset, it is imperative to treat TPN tubing with the utmost care. Avoid kinking, twisting, or bending the tubing excessively, as these actions can compromise its structural integrity and lead to premature failure. When disconnecting or reconnecting tubing, gently pull or push on the connectors, ensuring they are securely attached to prevent leaks or contamination.
Storage and Transportation
Proper storage and transportation are also vital for preserving the quality of TPN tubing. Store tubing in a cool, dry place, away from direct sunlight and extreme temperatures. When transporting tubing, securely wrap it to prevent damage and avoid placing heavy objects on top of it.
Regular Inspection
Regular inspection of TPN tubing is crucial for identifying any potential issues early on. Inspect the tubing carefully before each use, paying attention to signs of damage, leaks, or discoloration. If any irregularities are detected, discard the tubing immediately to prevent contamination or complications.
Cleaning and Sterilization
TPN tubing requires thorough cleaning and sterilization before each use. Refer to the manufacturer’s instructions for the specific cleaning and sterilization methods recommended for the type of tubing being used. Generally, cleaning involves flushing the tubing with a sterile solution, followed by sterilization using appropriate methods such as autoclaving or chemical disinfection.
Proper Priming
Priming TPN tubing is essential to remove any air bubbles and ensure proper flow of the TPN solution. Carefully follow the manufacturer’s instructions for priming the tubing and avoid introducing any air into the system during the process.
Adherence to Guidelines
Adhering to the manufacturer’s guidelines and established protocols for TPN tubing handling and maintenance is paramount. Regular changes, as recommended by the healthcare provider, are crucial for preventing complications and ensuring optimal patient outcomes.
By following these proper handling and maintenance techniques, healthcare professionals and patients can extend the lifespan of TPN tubing, minimize the frequency of changes, and enhance the safety and effectiveness of TPN therapy.
Importance of Timely TPN Tubing Changes for Patient Safety and Well-being
In the realm of Total Parenteral Nutrition (TPN), the integrity and timely replacement of tubing play a critical role in ensuring the safety and effectiveness of this life-sustaining therapy. Adhering to the recommended frequency of tubing changes is paramount for preventing complications and optimizing patient outcomes.
TPN tubing serves as a lifeline, delivering essential nutrients and fluids directly into the bloodstream. Maintaining the integrity of this tubing is crucial to prevent leaks, contamination, and the proliferation of microorganisms. Delayed or infrequent tubing changes can increase the risk of infection, malnutrition, and catheter-related issues.
Conversely, excessively frequent tubing changes can disrupt the delivery of nutrients, lead to electrolyte imbalances, and increase the risk of mechanical complications. Determining the optimal frequency of tubing changes is therefore essential and should be individualized based on several factors, including:
- Type of tubing (PVC-based or silicone-based)
- TPN solution composition
- Presence of additives
- Patient age, health status, and underlying conditions
Healthcare professionals should consult established guidelines and consult with the patient’s medical team to determine the appropriate frequency of tubing changes. By adhering to these recommendations, they can ensure that TPN therapy is delivered safely and effectively, promoting optimal patient outcomes.