Protein plays a crucial role in fluid balance by maintaining colloid osmotic pressure in blood. This pressure draws fluids from interstitial spaces into blood vessels, preventing excessive fluid accumulation in tissues. Protein also helps regulate hydrostatic pressure by controlling blood volume and preventing fluid leakage from blood vessels. Additionally, protein is involved in the lymphatic drainage and Renin-Angiotensin-Aldosterone System, which further contribute to fluid regulation.
Fluid Balance: The Foundation of a Healthy Body
- Importance of fluid balance in maintaining bodily functions and overall health.
Fluid Balance: The Foundation of a Healthy Body
In the symphony of life, fluid balance plays a harmonious tune, ensuring the seamless functioning of our bodies. Like a well-oiled machine, fluids nourish our cells, regulate temperature, and transport nutrients and waste. Maintaining a delicate equilibrium of fluids is paramount for our overall well-being.
Imagine your body as a tapestry woven with trillions of tiny cells. Each cell, a bustling metropolis, relies on a steady supply of fluids to thrive. These fluids act as messengers, carrying essential nutrients to fuel cellular activities and whisking away waste products.
Moreover, fluids regulate our body temperature, preventing us from overheating or freezing. Much like a thermostat, our bodies use fluids as a coolant, evaporating sweat through our skin to cool down when necessary.
Fluid balance also plays a crucial role in blood pressure regulation. Think of your blood vessels as a complex network of highways and byways. Fluids circulating through these vessels maintain the proper volume and pressure, ensuring that oxygen and nutrients reach every corner of our bodies.
Disruptions in fluid balance can lead to a cascade of health issues, such as dehydration, electrolyte imbalances, and even cardiovascular problems. Maintaining optimal fluid intake is therefore essential, especially during intense physical activity and in hot weather.
So, let us embark on a journey to understand the intricate workings of fluid balance, the foundation upon which a healthy body thrives.
Starling Forces and the Movement of Fluids
Our bodies are composed of approximately 60% fluid, which plays an indispensable role in virtually every bodily function, from nutrient delivery and waste removal to temperature regulation. The intricate movement of fluids between blood vessels and interstitial spaces (the spaces between cells) is governed by a delicate balance of forces known as Starling forces. These forces ensure the proper distribution of fluids throughout the body.
Gibbs-Donnan Effect: A Force to be Reckoned With
The Gibbs-Donnan effect is a phenomenon that occurs when there is a difference in the concentration of charged particles (ions) across a semipermeable membrane. In the context of fluid balance, this membrane is the capillary wall. The effect causes water to move from an area where there is a higher concentration of charged particles (such as sodium ions) to an area where there is a lower concentration, thereby maintaining electrical neutrality. This movement of water helps distribute fluids and solutes evenly.
Hydrostatic Pressure and Colloid Osmotic Pressure: A Balancing Act
Hydrostatic pressure is the force exerted by a fluid due to its height. In the circulatory system, hydrostatic pressure is generated by the heart’s pumping action. Colloid osmotic pressure, on the other hand, is the force exerted by large molecules (such as proteins) that cannot cross the capillary wall.
Inside a capillary, hydrostatic pressure promotes the movement of fluids from the blood into the interstitial space. However, colloid osmotic pressure exerts an opposing force, drawing fluids back into the blood. The balance between these two forces determines the net movement of fluids. In normal conditions, the colloid osmotic pressure is slightly higher than the hydrostatic pressure, favoring fluid movement into the blood.
Starling Forces in Action: Keeping Fluid Balance in Check
Starling forces are crucial in maintaining fluid balance. If the Starling forces are not balanced, fluid can accumulate in interstitial spaces, leading to edema (swelling). Conversely, if the colloid osmotic pressure is too low, fluid can leak out of the blood vessels into the interstitial spaces, leading to dehydration.
Understanding the Gibbs-Donnan effect, hydrostatic pressure, and colloid osmotic pressure is essential for comprehending the complex interplay of forces that govern fluid balance in our bodies. These forces ensure that fluids are distributed and utilized efficiently, supporting countless physiological processes and maintaining our overall well-being.
Colloid Osmotic Pressure and Hydrostatic Pressure: The Balancing Act
- Colloid osmotic pressure: its contribution to fluid balance and its role in maintaining the integrity of blood vessels.
- Hydrostatic pressure: its role in fluid movement and the regulation of blood volume.
Colloid Osmotic Pressure and Hydrostatic Pressure: A Balancing Act in Fluid Regulation
In a healthy body, a delicate dance of fluids occurs, maintaining a harmonious equilibrium that sustains life. Two key players in this fluid ballet are colloid osmotic pressure and hydrostatic pressure. Understanding their roles in fluid balance is crucial for overall well-being.
Colloid Osmotic Pressure: The Warden of Blood Vessel Integrity
Imagine your blood vessels as tiny rivers coursing through your body. These rivers contain plasma, a liquid that carries essential substances, including proteins. Proteins, being large molecules, cannot easily cross the vessel walls. This creates a concentration gradient, where the protein concentration is higher inside the vessels than outside.
This concentration gradient generates a force known as colloid osmotic pressure. It acts like an invisible barrier, drawing water molecules from the interstitial space (the area outside the vessels) into the blood vessels. This inward pull helps maintain proper fluid balance and prevents fluid from leaking out of the vessels.
Hydrostatic Pressure: Regulating Blood Volume
Hydrostatic pressure, on the other hand, is the force exerted by a column of fluid. In our circulatory system, it refers to the pressure exerted by the blood within the vessels. As blood flows through the vessels, hydrostatic pressure changes.
At the arterial end (where blood is pumped out of the heart), hydrostatic pressure is high. This pressure pushes fluid out of the vessels and into the interstitial space. At the venous end (where blood returns to the heart), hydrostatic pressure is lower, favoring fluid reabsorption back into the vessels.
The Symphony of Fluid Regulation
Colloid osmotic pressure and hydrostatic pressure work together in a beautiful symphony to regulate fluid balance. Colloid osmotic pressure draws fluid in, while hydrostatic pressure pushes fluid out. This delicate balancing act ensures that the right amount of fluid is circulating in the blood vessels and interstitial space, supporting vital bodily functions.
The intricate relationship between colloid osmotic pressure and hydrostatic pressure underscores the remarkable complexity of our bodies. Understanding these concepts allows us to appreciate the intricate choreography that maintains our fluid balance and overall health.
The Lymphatic System: A Drainage Master for Fluid Balance
Just as a drainage system is crucial for any household, the lymphatic system plays a vital role in your body’s plumbing. This intricate network of vessels, nodes, and organs works tirelessly to drain excess fluids, maintaining a delicate balance that is essential for your overall health.
The lymphatic system acts as a parallel circulatory system, collecting interstitial fluid—the fluid that surrounds your cells. This fluid contains waste products, bacteria, and other substances that need to be eliminated. As the lymphatic vessels absorb this fluid, they filter out these unwanted elements, allowing them to be transported to lymph nodes for further processing.
The lymph nodes, scattered throughout your body, act as checkpoints, trapping bacteria and other harmful substances. As the fluid passes through these nodes, it is cleaned, and the impurities are destroyed by immune cells. The cleansed fluid is then returned to the bloodstream via lymphatic ducts.
The lymphatic system’s role is intricately intertwined with two other key players in fluid balance: the Renin-Angiotensin-Aldosterone System (RAAS) and Antidiuretic Hormone (ADH). RAAS helps to regulate blood pressure and fluid volume, while ADH controls water reabsorption in the kidneys.
When the lymphatic system efficiently drains excess fluids, it works in harmony with RAAS and ADH to maintain the body’s fluid balance. Proper fluid balance is essential for optimal organ function, waste elimination, and overall well-being.
So, the next time you think about drainage, remember the unsung hero of your body—the lymphatic system. It’s the tireless drainage master, ensuring your bodily fluids flow smoothly, keeping you healthy and hydrated.
The Renin-Angiotensin-Aldosterone System: A Vital Regulator of Blood Pressure and Fluid Balance
The human body is an intricate web of interconnected systems, each playing a crucial role in maintaining homeostasis. Among these systems, the Renin-Angiotensin-Aldosterone System (RAAS) stands out as a master regulator of blood pressure and fluid balance. Let’s unravel the fascinating story of RAAS and its impact on our overall health.
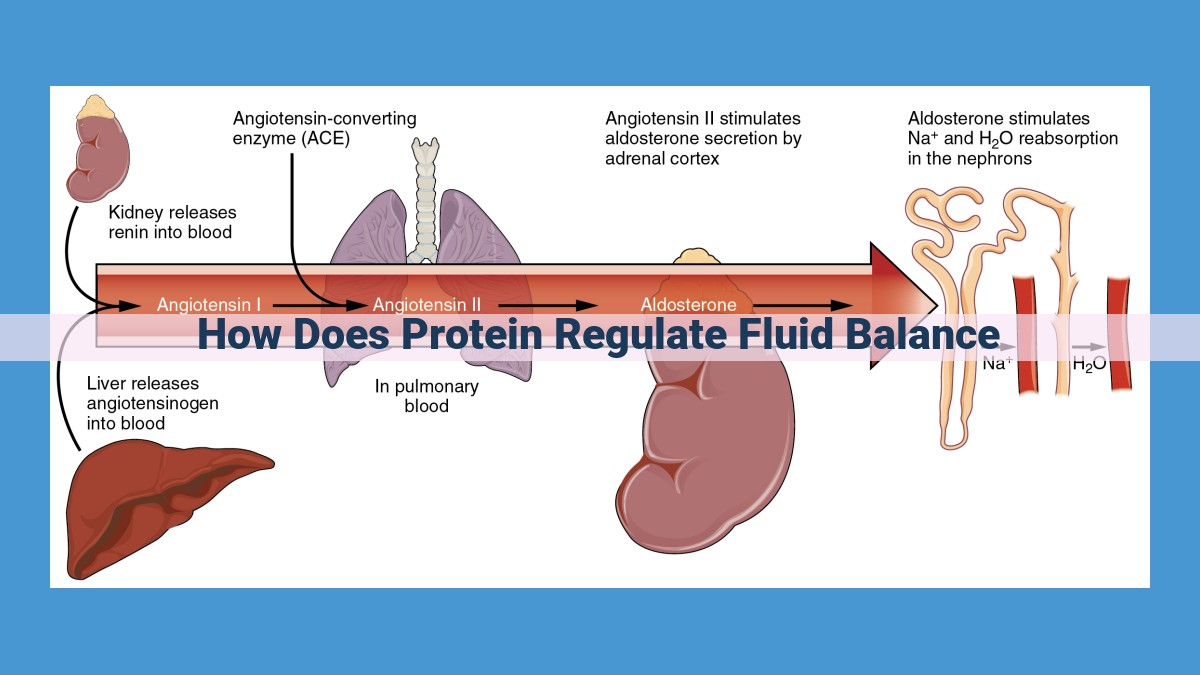
RAAS is a complex hormone signaling pathway that kicks into action when blood pressure drops or blood volume decreases. The kidneys, sensing these changes, release an enzyme called renin. Renin converts a protein in the blood called angiotensinogen into angiotensin I. Angiotensin I is then further converted into angiotensin II by an enzyme found in the lungs.
Angiotensin II is the star of the RAAS show. It has two primary functions:
- Vasoconstriction: Angiotensin II causes blood vessels to narrow, which increases blood pressure.
- Aldosterone release: Angiotensin II stimulates the adrenal glands to release aldosterone, a hormone that promotes sodium reabsorption in the kidneys. This increased sodium reabsorption leads to water retention, which increases blood volume.
By adjusting these two factors, RAAS helps maintain optimal blood pressure and fluid balance.
However, RAAS is not an isolated player. It interacts closely with the lymphatic system, a network of vessels that drain excess fluid from tissues and return it to the bloodstream. The lymphatic system helps remove fluid that accumulates due to increased blood pressure.
Additionally, RAAS interacts with Antidiuretic Hormone (ADH), which regulates water reabsorption in the kidneys. When blood pressure or fluid volume decreases, ADH is released, promoting water retention and further contributing to fluid balance.
In essence, RAAS, the lymphatic system, and ADH form a triumvirate of regulators that work in concert to maintain the body’s intricate fluid balance and blood pressure. It is through these sophisticated mechanisms that our bodies strive to achieve and sustain a state of equilibrium, ensuring optimal function and overall well-being.
Antidiuretic Hormone: The Water Guardian
Maintaining fluid balance is crucial for our bodies to function optimally. Antidiuretic hormone (ADH), also known as vasopressin, plays a pivotal role in this delicate equilibrium. Produced by the pituitary gland, ADH regulates water reabsorption in the kidneys, ensuring that our bodies retain the necessary fluid.
When the body senses a decrease in blood volume or an increase in blood osmolality(concentration of solutes), ADH is released. It travels to the kidneys and binds to receptors in the collecting ducts, increasing their permeability to water. This allows water to reabsorb back into the bloodstream, reducing urine output and conserving fluid.
ADH also interacts with the lymphatic system and the renin-angiotensin-aldosterone system (RAAS) to maintain fluid balance. The lymphatic system collects excess fluid from tissues and transports it back into the bloodstream. RAAS, on the other hand, regulates blood pressure and fluid volume by constricting blood vessels and stimulating the release of aldosterone, which increases water and sodium reabsorption in the kidneys.
ADH works in concert with lymph nodes and hormones from the RAAS to ensure that water retention and excretion are in sync with the body’s fluid needs. This complex interplay helps maintain stable blood volume, optimizes blood pressure, and prevents dehydration.
In summary, antidiuretic hormone is a crucial regulator of water balance in the body. It directly affects kidney function and interacts with other systems to ensure that we have the right amount of fluid to support our health and well-being. By understanding the role of ADH, we can appreciate the intricate mechanisms that keep us hydrated and healthy.
Protein: The Key to Maintaining Proper Fluid Balance
Understanding the Importance of Fluid Balance
Fluid balance is crucial for maintaining optimal bodily functions and overall health. Our body consists of approximately 60% water, which is distributed throughout various compartments, including blood, interstitial spaces, and cells. Maintaining a proper balance of fluids in these compartments is essential for:
- Regulating body temperature
- Transporting nutrients and waste products
- Protecting sensitive tissues
- Maintaining blood pressure
The Role of Protein in Fluid Regulation
Protein plays a vital role in controlling fluid balance by maintaining what is known as colloid osmotic pressure. Colloid osmotic pressure (COP) is the pressure exerted by proteins within the blood vessels that helps to pull water into the bloodstream.
Normally, protein is present in the blood in quantities that create a higher COP within the blood vessels compared to the interstitial spaces. This pressure gradient favors the movement of water into the blood vessels, preventing fluid build-up in tissues and maintaining a healthy fluid balance.
Summary of Fluid Regulation
The intricate network of fluid movement in our body is influenced by various factors, including:
- Starling forces: Hydrostatic and colloid osmotic pressures governing fluid exchange between blood vessels and interstitial spaces.
- Lymphatic system: Draining excess fluid and returning it to the bloodstream.
- Renin-Angiotensin-Aldosterone System (RAAS): Regulating blood pressure and influencing fluid balance.
- Antidiuretic Hormone (ADH): Controlling water reabsorption in the kidneys to maintain fluid volume.
The Significance of Protein
In the context of these regulatory mechanisms, protein stands out as a key factor in fluid balance. Adequate intake of protein maintains proper colloid osmotic pressure within blood vessels, which prevents excessive fluid leakage into tissues. This ensures the availability of sufficient fluid volume in the bloodstream to meet the body’s physiological needs.
Therefore, consuming an adequate amount of high-quality protein is essential for maintaining proper fluid balance, supporting optimal bodily functions, and promoting overall health.