The complement pathway, a crucial part of the immune system, targets and destroys pathogens. Cytolysis, induced via the complement pathway, is the lysis of target cells by the membrane attack complex (MAC). The MAC inserts into the cell membrane, creating pores that lead to cell lysis. The complement pathway’s sequential activation of complement proteins, involving C3 convertase and C5 convertase, triggers MAC formation. Additionally, the complement system contributes to pathogen elimination by opsonization for phagocytosis, inflammation through anaphylatoxin release, and cell recruitment via chemotaxis and degranulation. Understanding the mechanisms of complement activation and its related concepts is vital for comprehending immune defense and inflammatory responses.
The Complement Pathway: A Mighty Defender in Your Body’s Immune Arsenal
Your body’s immune system is a remarkable guardian, constantly on the lookout for invaders that threaten your well-being. Among its arsenal of weapons is the complement pathway, a complex network of proteins that plays a crucial role in eliminating pathogens and defending your health.
Cytolysis is a vital process in this defense strategy. It involves poking holes in the membranes of target cells, such as bacteria or infected cells, causing them to burst and die. The complement pathway is a master at orchestrating cytolysis, using a series of sequential steps to neutralize and destroy intruders.
The Complement Pathway
- Describe the three pathways that activate the complement pathway: classical, alternative, and lectin.
- Explain the sequential activation of complement proteins.
The Complement Pathway: Unveiling the Body’s Silent Sentinel
In the realm of the immune system, there exists a powerful and intricate web of defense mechanisms working tirelessly to protect our bodies from invading pathogens. Among these mechanisms, the complement pathway stands out as a crucial player in eliminating harmful microorganisms and ensuring our well-being.
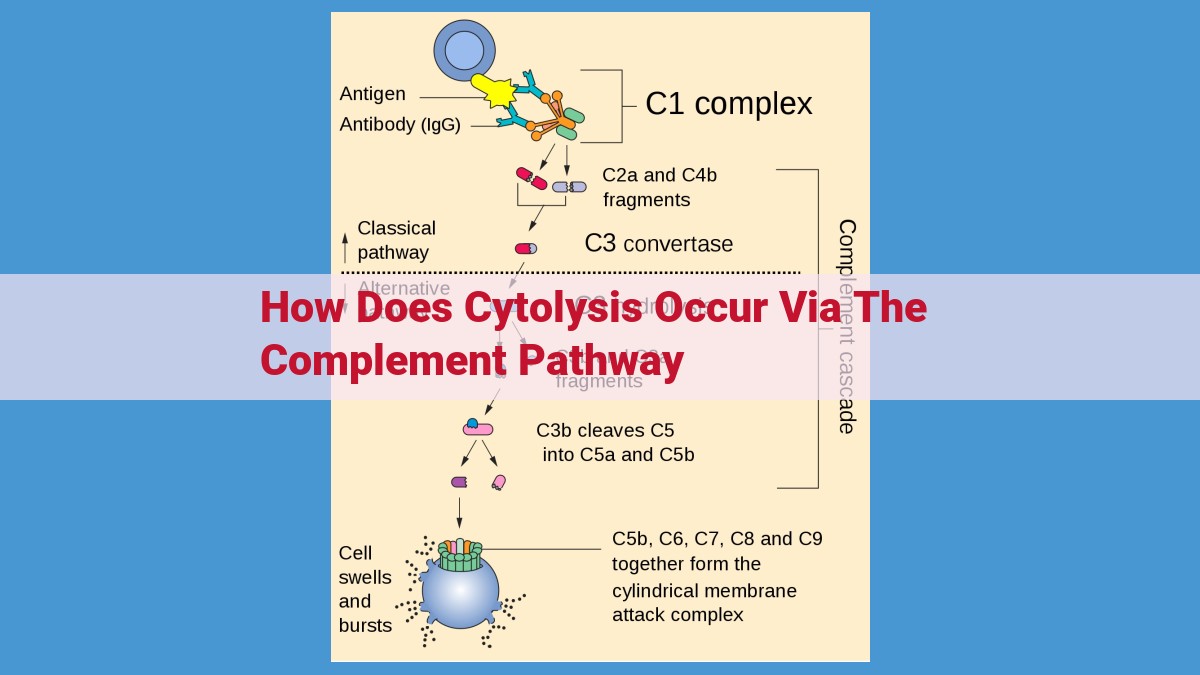
The complement pathway is a complex cascade of proteins that, when activated, leads to the destruction of pathogens through a process called cytolysis. This pathway can be triggered through three distinct routes:
1. The Classical Pathway:
This pathway is initiated by the binding of antibodies to specific antigens on the surface of a pathogen. These antibodies act as beacons, signaling to complement proteins to attack the target.
2. The Alternative Pathway:
Unlike the classical pathway, this route involves a direct interaction between complement proteins and bacterial cell walls or viral envelopes. It amplifies the response and provides a broader defense against pathogens.
3. The Lectin Pathway:
Similar to the alternative pathway, the lectin pathway utilizes proteins called lectins to recognize and bind to carbohydrates on the surface of pathogens, triggering the complement cascade.
Once any of these pathways is activated, a sequential activation of complement proteins ensues. These proteins interact with each other in a carefully orchestrated manner, forming complexes that amplify the signal and lead to the ultimate destruction of the pathogen.
Cytolysis via the Complement Pathway: The Lethal Blow in Immune Defense
The complement pathway, an essential component of our immune system, plays a crucial role in eliminating pathogens and safeguarding our health. One of its key mechanisms is cytolysis, the destruction of target cells via a specialized molecular complex known as the membrane attack complex (MAC).
Formation of the Membrane Attack Complex (MAC)
The formation of the MAC is a carefully choreographed process initiated by the activation of specific complement proteins. C5 convertase, an enzyme complex, plays a pivotal role in this process. It cleaves the complement protein C5 into two fragments, C5a and C5b. C5b, combined with additional complement proteins, forms the core of the MAC.
Role of C5b and C5 Convertase
C5b serves as the foundation upon which the MAC is assembled. It anchors itself to the target cell membrane and recruits a series of other complement proteins, including C6, C7, C8, and ultimately C9. These proteins form a ring-like structure that embeds itself within the target cell membrane.
Insertion of the MAC and Cell Lysis
The insertion of the MAC into the target cell membrane causes a critical disruption. C9 polymerizes, creating a transmembrane channel that allows the influx of ions and water into the cell. This leads to cell swelling, osmotic rupture, and ultimately cytolysis, or cell death.
The complement pathway’s ability to lyse target cells is a vital defense mechanism against pathogens. It helps eliminate bacteria, viruses, and other infectious agents that may pose a threat to our health. Understanding the mechanisms of complement activation and its related concepts is crucial for appreciating the body’s intricate immune defense system.
Related Concepts: The Complement Pathway and Immune Defense
Opsonization: Tagging Pathogens for Elimination
The complement pathway plays a crucial role in opsonization, a process where specific proteins called complement proteins tag pathogens, making them more easily recognized and engulfed by immune cells. Complement proteins bind to the surface of pathogens, creating a molecular beacon that attracts phagocytes, such as macrophages and neutrophils. Once tagged, pathogens become easier targets for engulfment and subsequent destruction.
Phagocytosis: Engulfing and Destroying Pathogens
Phagocytosis is the process by which phagocytes engulf and destroy pathogens. These immune cells recognize and attach to opsonized pathogens, extending their membrane to engulf and form a phagosome, which encapsulates the pathogen. The phagosome then fuses with a lysosome, an organelle containing digestive enzymes, to form a phagolysosome. Within the phagolysosome, the pathogen is broken down and destroyed, eliminating the infection.
Inflammation: A Coordinated Defense Response
The complement pathway also contributes to inflammation, a localized response to injury or infection. When complement proteins are activated, they release molecules called anaphylatoxins, which trigger the inflammatory response. Anaphylatoxins cause blood vessels to dilate, increasing blood flow to the affected area. They also attract neutrophils and other immune cells to the site of infection.
C3 and C5 Convertases: Key Enzymes in the Complement Cascade
C3 convertase and C5 convertase are two crucial enzymes in the complement cascade. C3 convertase cleaves complement protein C3 into two fragments, C3a and C3b. C3b opsonizes pathogens, while C3a acts as an anaphylatoxin. C5 convertase, on the other hand, cleaves C5 into C5a and C5b. C5a is another anaphylatoxin, while C5b initiates the formation of the membrane attack complex (MAC).
Anaphylatoxins, Chemotaxis, and Degranulation: Mediators of the Inflammatory Response
Anaphylatoxins, such as C3a and C5a, play a significant role in the inflammatory response. They activate mast cells and basophils, causing the release of histamine and other inflammatory mediators. Histamine promotes vasodilation and increased permeability of blood vessels, allowing immune cells and fluid to enter the infected area. Chemotaxis refers to the movement of immune cells towards a chemical gradient, and anaphylatoxins serve as chemotactic agents, guiding immune cells to the site of infection. Additionally, anaphylatoxins trigger degranulation, the release of antimicrobial substances from neutrophils and macrophages, directly killing pathogens and contributing to tissue damage.